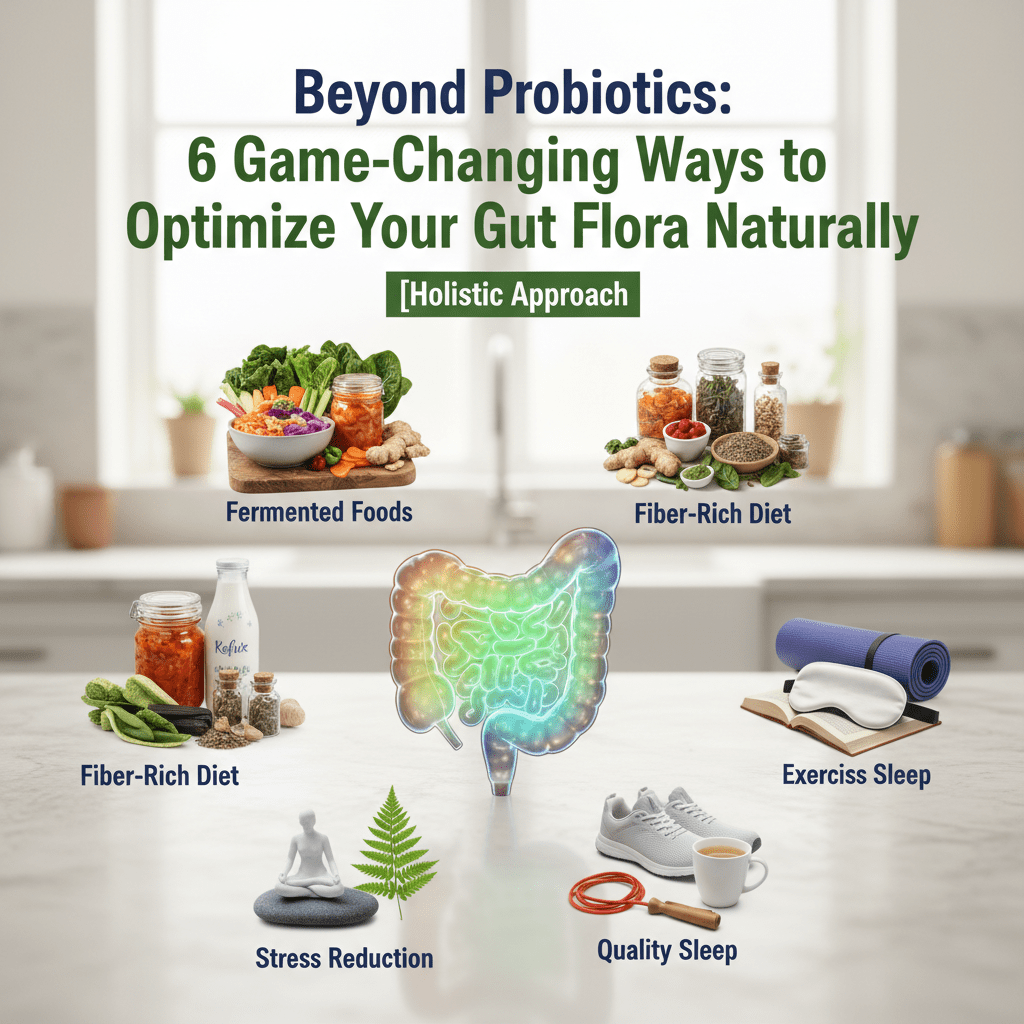
Beyond Probiotics: 6 Game-Changing Ways to Optimize Your Gut Flora Naturally [Holistic Approach]
Taking a probiotic pill to fix a damaged gut is like throwing premium grass seeds onto a concrete parking lot. You might get a sprout or two, but without changing the “soil”—your internal environment—nothing is going to take root.
In my years analyzing health trends and nutritional data, I’ve seen countless people cycle through expensive supplements, hoping to fix their bloating, brain fog, or immune issues. Yet, the data is sobering. According to a Dec 2024 report from the NIH, digestive diseases now account for 472,000 deaths annually in the U.S. alone. If pills were the answer, those numbers would be dropping, not rising.
The truth is, how to optimize gut flora naturally requires a shift from “supplementation” to “cultivation.” It’s about circadian rhythms, the physical tone of your nervous system, and the chemical signaling of your food.
I’ve combed through the latest 2024-2025 research from institutions like Stanford, UCLA, and King’s College London to bring you six non-negotiable, pill-free protocols. These aren’t just old wives’ tales; they are the new science of the microbiome.


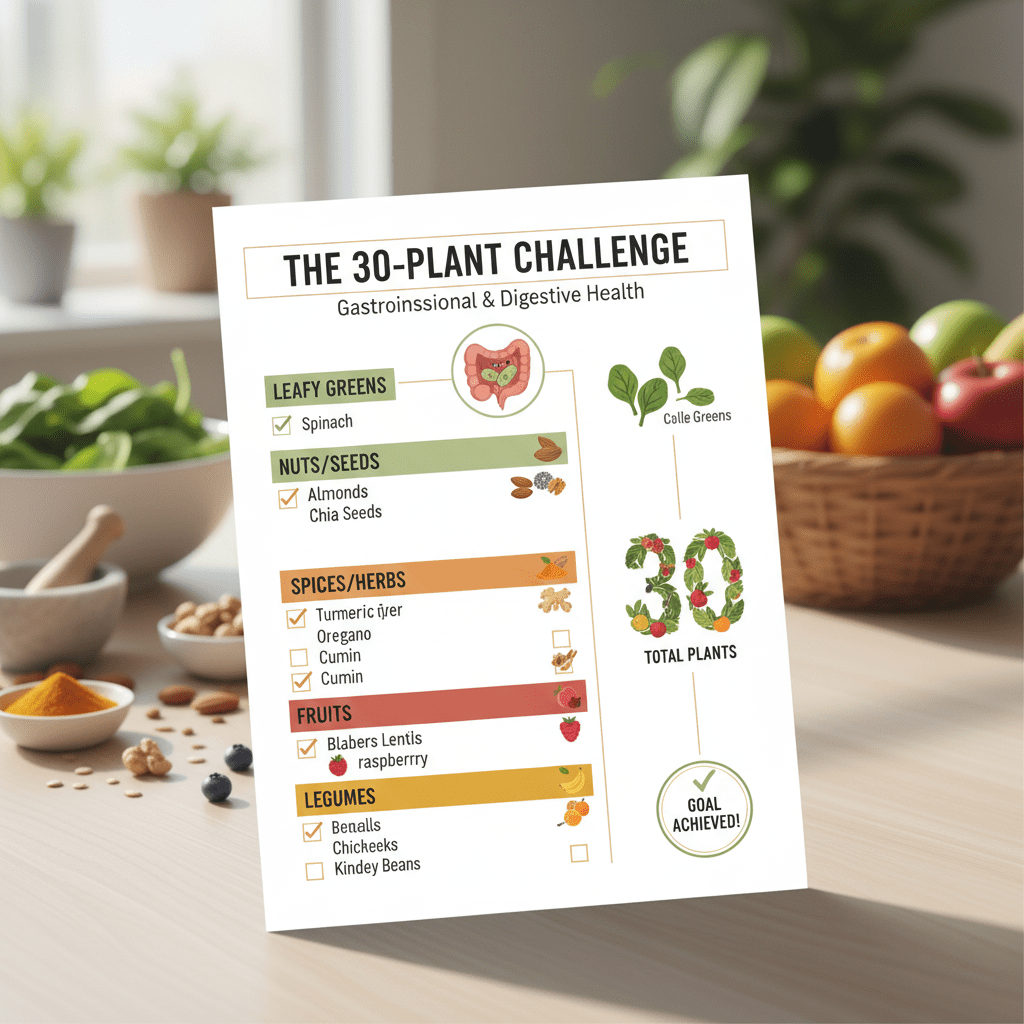
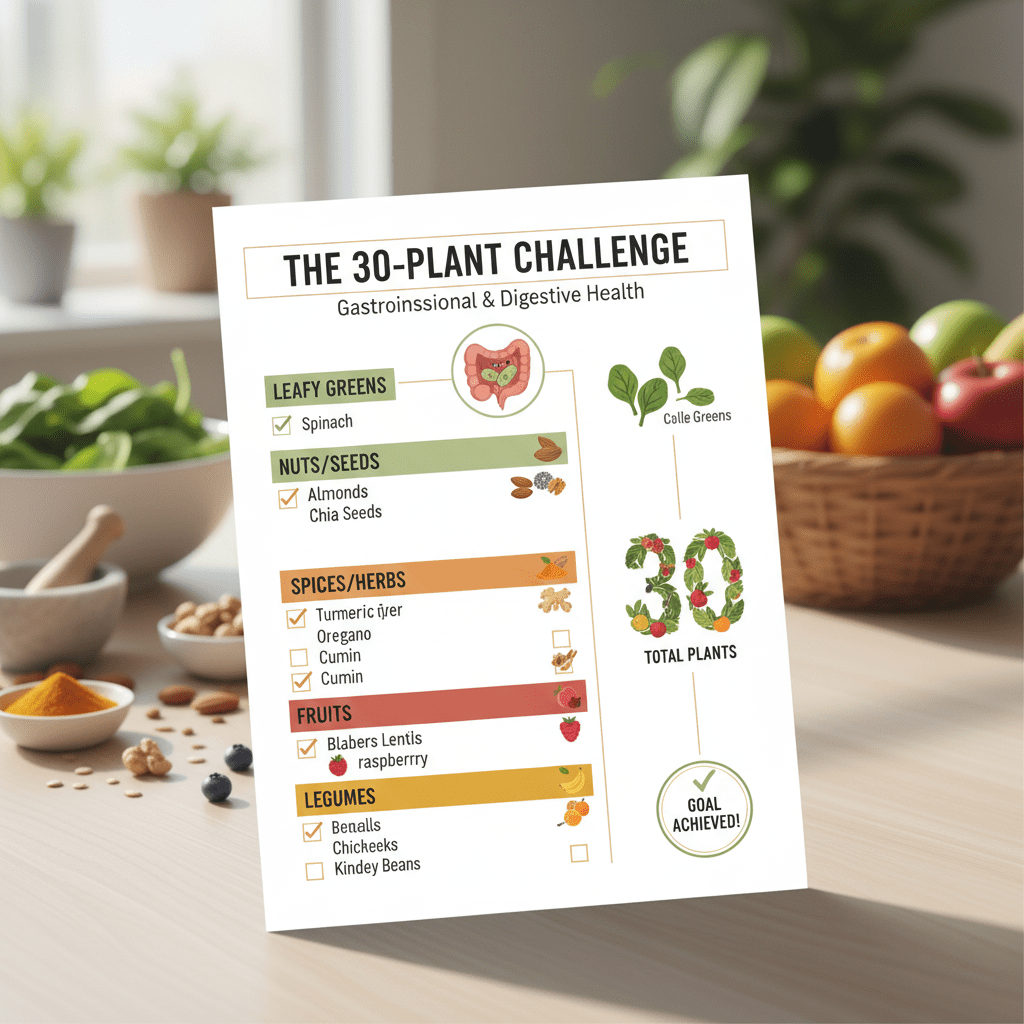
1. The “30-Plant” Protocol: Diversity is the New Superfood
If you take nothing else from this article, take this: Diversity determines resilience.
For decades, we obsessed over “good” vs. “bad” bacteria. But recent insights from the American Gut Project suggest that the number of different bacterial species matters more than simply having a lot of Lactobacillus. This is where microbiome diversity comes into play.
According to Dr. Tim Spector of ZOE, the magic number is 30. His research indicates that individuals who consume 30 or more different types of plants per week have significantly more diverse microbiomes than those who eat 10 or fewer.
of Americans do not meet the recommended daily fiber intake, starving their beneficial bacteria.
It sounds daunting, doesn’t it? But here’s the trick I use with clients: It’s not just about vegetables. In the world of gut health, a “plant” is anything that grows from the ground.
How to Hit Your 30 Points
To optimize gut flora naturally, you need to expand your definition of plant-based. Here is how you can rack up points quickly:
- Herbs & Spices: A teaspoon of oregano counts. A sprinkle of cinnamon counts. (These are packed with polyphenols).
- Nuts & Seeds: Almonds, chia seeds, walnuts, and pumpkin seeds all count as separate plants.
- Legumes: Chickpeas, lentils, black beans.
- Whole Grains: Oats, quinoa, buckwheat.
If you eat a salad with spinach, arugula, cucumber, tomato, pumpkin seeds, and a dressing made with olive oil and lemon juice, you’ve just hit 7 plants in one meal. It’s about variety, not volume.
2. Circadian Syncing: Time Your Meals to Your Microbes
This is the most overlooked aspect of gut health. We often ask what to eat, but rarely when to eat. However, a Feb 2024 systematic review in Frontiers in Nutrition confirmed that Time-Restricted Eating (TRE) significantly improves the *Firmicutes/Bacteroidetes* ratio and restores healthy circadian gene expression in the gut.
Here is the thing: Your gut bacteria have a bedtime. Just like you, they need a rest phase to repair and reproduce.
The “Migrating Motor Complex” (MMC)
When you are in a fasted state (usually 3-4 hours after your last meal), a cleaning wave known as the Migrating Motor Complex sweeps through your intestines. It pushes undigested food and bacteria from the small intestine into the colon.
If you are constantly grazing or snacking late at night, you stop this cleaning crew from doing its job. This is a leading cause of SIBO (Small Intestinal Bacterial Overgrowth) and general dysbiosis.
3. The “Matrix” Effect: Why Fermented Foods Beat Pills
I often get asked, “Why can’t I just take a probiotic?” The answer lies in the “Food Matrix.” A pill is often just bacteria in a capsule, vulnerable to stomach acid and heat. Fermented foods, however, provide a protective matrix of proteins, fats, and fibers that help the bacteria survive the journey to your colon.
The science backing this is incredibly strong. A landmark study from Stanford Medicine (Sonnenburg/Gardner) compared a high-fiber diet to a high-fermented-food diet. The results were shocking.
While fiber is essential, the study found that fermented foods increased microbiome diversity and decreased 19 inflammatory markers (including IL-6) more effectively than fiber alone in the short term. Dr. Justin Sonnenburg noted that the mice fed a Western diet retained a fraction of diversity, but fermented foods acted as a rehabilitation tool.
The “Fermented Fork” Rule
You don’t need to eat a bowl of sauerkraut. You just need a “forkful” daily. Incorporate these naturally:
- Kefir: Contains up to 60 strains of bacteria (yogurt usually has 2-4).
- Kimchi: Loaded with fiber and Lactobacillus.
- Miso: Great for soups and dressings.
- Sauerkraut: Look for “raw” or “unpasteurized” in the refrigerated section.


4. Vagus Nerve Activation: The Physical Switch for Digestion
This is where we move completely beyond diet. The gut-brain axis is a physical connection, primarily facilitated by the Vagus nerve. It’s the superhighway that tells your gut to produce enzymes and move food along (motility).
If you are stressed, your body is in “fight or flight” mode. In this state, the Vagus nerve shuts down digestion. You can eat the perfect 30-plant diet, but if your Vagus nerve is dormant, you won’t absorb the nutrients properly.
A groundbreaking Feb 2025 study by Jameson et al. at UCLA proved a direct causal link: specific microbial metabolites in the intestine physically activate the Vagus nerve to send “calm” signals to the brain. It’s a two-way street.
2-Minute Vagus Toning Exercises
You can manually stimulate this nerve to improve gut motility:
- Humming or Chanting: The Vagus nerve passes through the vocal cords. Deep humming creates vibrations that stimulate the nerve.
- Cold Water Splash: Splashing freezing water on your face stimulates the “dive reflex,” instantly increasing Vagal tone.
- Deep Diaphragmatic Breathing: Slow exhales (longer than inhales) switch your body from sympathetic (stress) to parasympathetic (digest/rest).
5. Polyphenol Loading: Feed Your *Akkermansia*
There is a specific bacterium gaining fame in the medical community called Akkermansia muciniphila. It is associated with a strong gut lining and leanness. The problem? It’s very hard to take as a probiotic supplement because it’s an anaerobe (it dies in oxygen).
So, how do you get it? You have to feed it.
According to research published in Antioxidants (Oct 2024), dietary polyphenols act as prebiotics that specifically boost Akkermansia levels. The study found that polyphenols from pomegranates and cranberries could increase abundance by up to 300%.
Polyphenols are the compounds that give foods their dark red, blue, and purple colors. They are “rocket fuel” for your good bacteria.
The “Dark” Diet Checklist:
- Blackberries and Blueberries
- Black Rice (Forbidden Rice)
- Dark Chocolate (85% cocoa or higher)
- Green Tea (Matcha is best)
- Red onions


6. Environmental Detox: Removing the “Microbiome Killers”
Finally, we have to talk about what you need to remove. You can’t heal a wound if you keep picking at it. In our modern environment, we are ingesting compounds daily that act as “antibiotics” to our good flora.
The Business Research Company’s 2025 report highlights that the rise in digestive health issues correlates directly with the consumption of ultra-processed foods. But specifically, what are the culprits?
The Hidden Saboteurs
- Emulsifiers (Polysorbate-80 & CMC): Found in shelf-stable nut milks, ice creams, and sauces. Studies show these strip away the mucus layer of the gut, leading to “leaky gut” or intestinal permeability.
- Chlorinated Water: Chlorine is added to tap water to kill bacteria. It does a great job—but it doesn’t distinguish between the bad bacteria in the pipes and the good bacteria in your gut. A simple carbon filter can remove this.
- NSAIDs: Chronic use of ibuprofen or aspirin is well-documented to damage the gut lining.
In my opinion, filtering your drinking water is the single highest-ROI change you can make for your gut health today. It’s a one-time cost for a daily protective benefit.
Frequently Asked Questions (FAQ)
While changes in bacterial composition can happen in as little as 24-48 hours after a drastic diet change, lasting remodeling and healing of the gut lining typically takes 4 to 6 weeks of consistent habit change. It is a biological process, not a mechanical fix.
Beyond antibiotics, the biggest natural killers of gut diversity are chronic stress (cortisol), lack of sleep, alcohol, and a diet high in refined sugar and artificial sweeteners. Environmental toxins like pesticides (glyphosate) also disrupt the microbiome.
Yes. As mentioned in the Circadian Syncing section, intermittent fasting (12-16 hours) allows the Migrating Motor Complex to clean the gut, preventing bacterial overgrowth in the small intestine and reducing systemic inflammation.
Start with the “Remove and Replace” method. Remove inflammatory triggers (sugar, alcohol, emulsifiers). Replace them with fermented foods, a diverse range of 30+ plants per week, and practice stress-reduction techniques to activate the Vagus nerve.
Conclusion: It’s a Lifestyle, Not a Pill
Optimizing your gut flora naturally isn’t about finding the perfect probiotic strain on Amazon. It’s about recreating the environment your microbiome evolved to thrive in: diverse, rhythmic, and chemical-free.
As Dr. Erica Sonnenburg from Stanford eloquently put it, “99% of our genetic material is microbial in origin. If you really want to get to a human genome, you have to understand all the bacteria.”
Your Next Step: Don’t try to do all six protocols at once. Start this week with the 30-Plant Challenge. Print out a list, stick it on your fridge, and treat it like a game. Your gut—and your long-term health—will thank you.