Conquering Crohn’s & Colitis: 5 Breakthrough Treatments & Lifestyle Hacks [Inflammation Reversed]
For years, achieving “remission” with Inflammatory Bowel Disease (IBD) felt a lot like winning the lottery. You threw darts at a board—prednisone, mesalamine, maybe a biologic—and prayed the inflammation would subside before your quality of life did.
I’ve spoken to countless patients who lived in fear of the next flare. But as we move deep into 2025, the narrative is shifting. Remission is no longer about luck; it is becoming a calculated science.
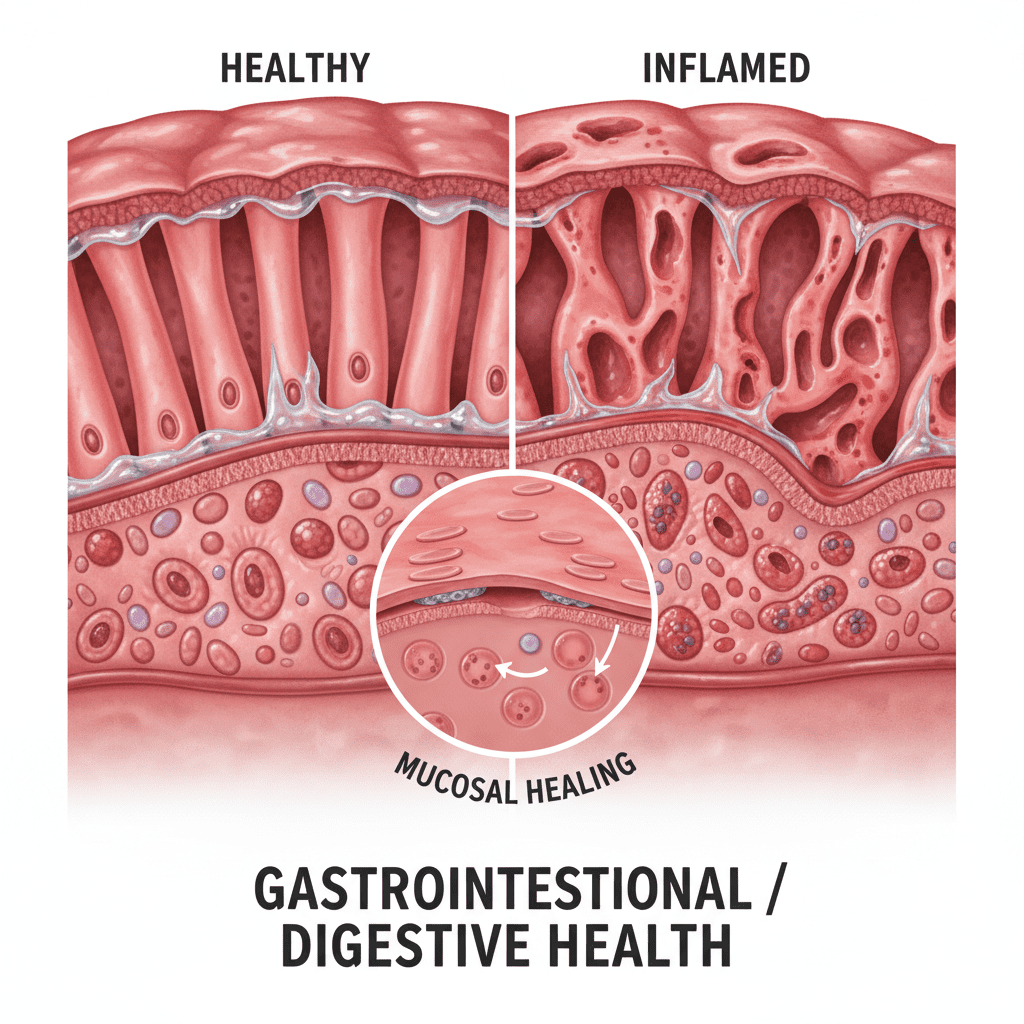
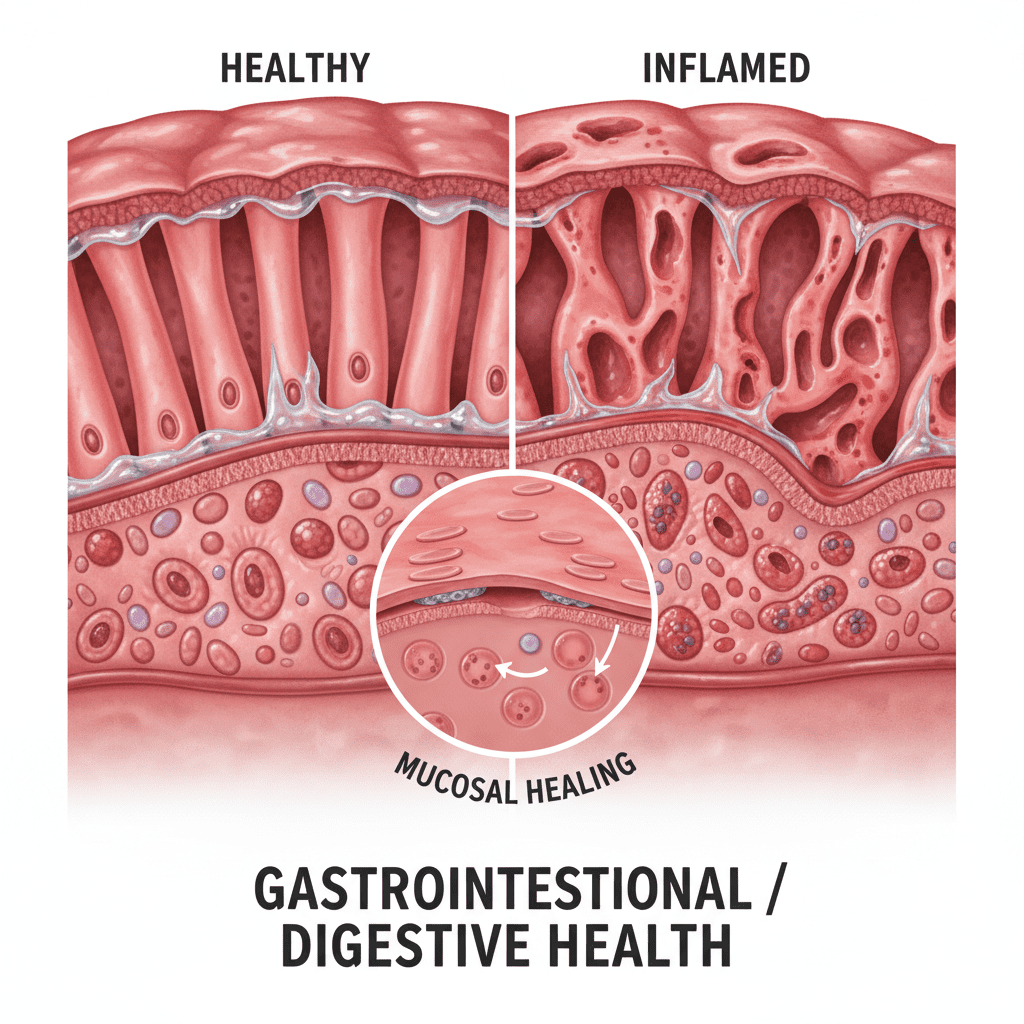
We are witnessing a paradigm shift from simple “symptom management” to “mucosal healing” and “histologic remission”—actually healing the gut tissue under a microscope. The data coming out of late 2024 and early 2025 is staggering. We aren’t just suppressing immune systems anymore; we are targeting specific pathways with laser precision.
In this guide, we are going to break down the “Heavy Artillery”—the medical breakthroughs dominating the 2025 landscape—and pair them with the “Daily Defense,” lifestyle hacks backed by hard statistics that you can start today.
The “Heavy Artillery”: 5 Medical Breakthroughs (2024-2025)
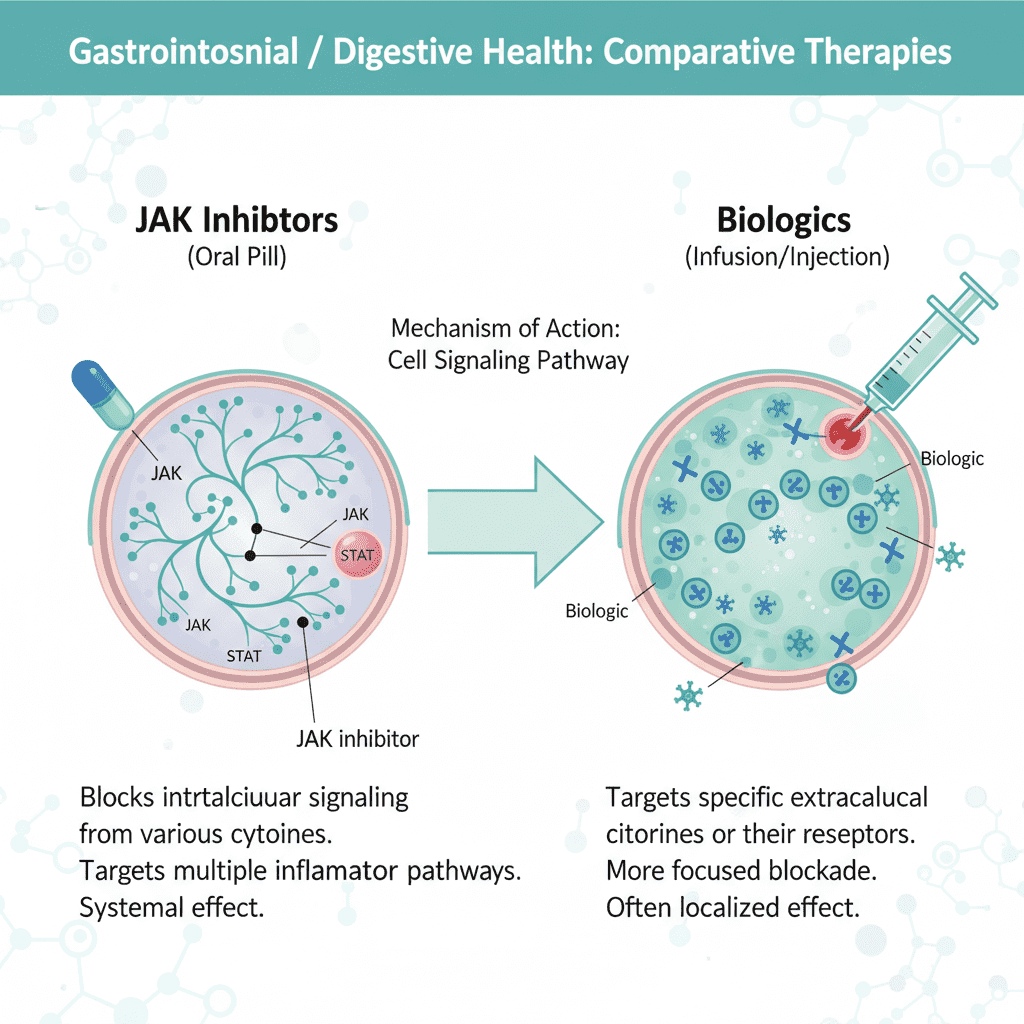
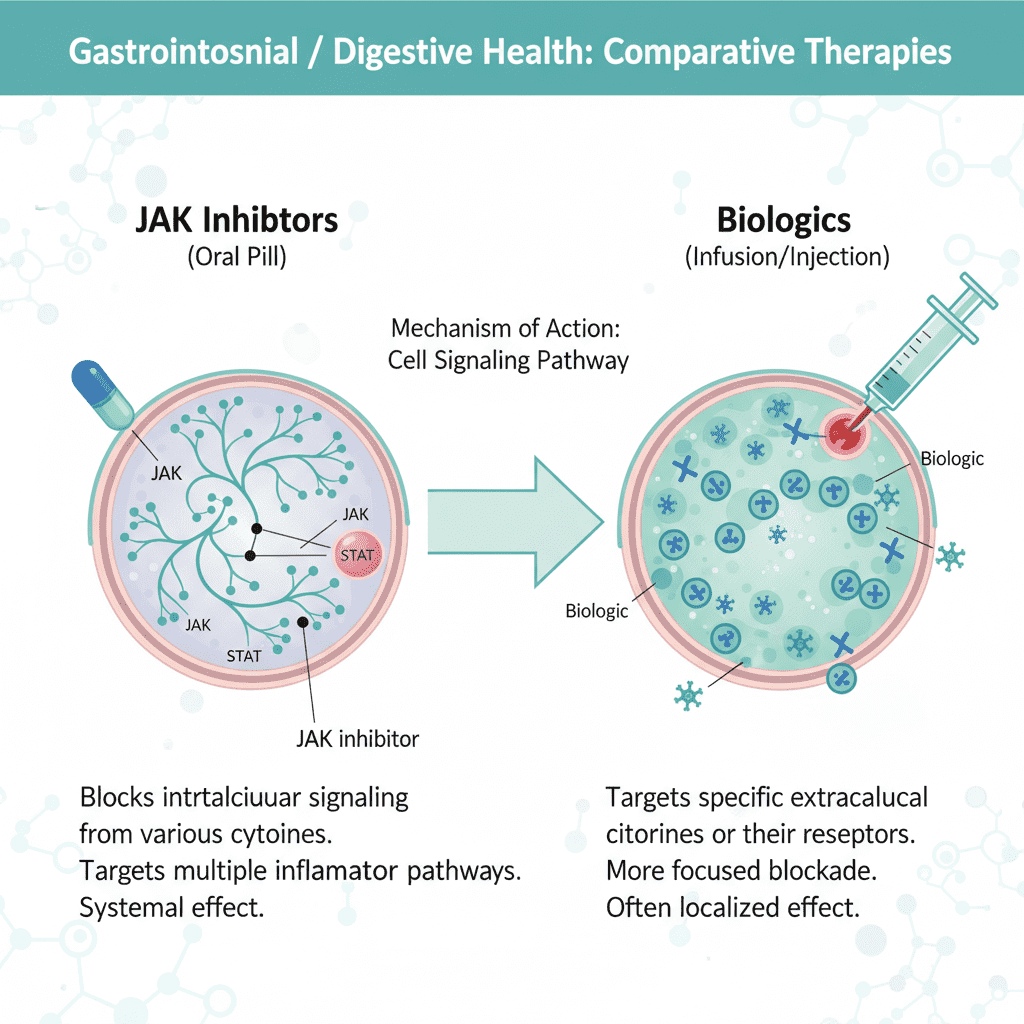
The days of a “one-size-fits-all” approach to Crohn’s and Colitis are fading. The new wave of therapies targets specific proteins (like IL-23) and pathways (like JAK and S1P) to stop inflammation at the source without necessarily shutting down your entire immune system.
1. Mirikizumab (Omvoh): The “Bowel Urgency” Stopper
If you have Ulcerative Colitis or Crohn’s, you know that pain isn’t always the worst symptom. It’s the urgency—the panic of needing a restroom now. For a long time, clinical trials ignored this metric. That has changed with Mirikizumab.
Mirikizumab is an IL-23p19 antagonist. In plain English, it blocks a specific protein that fuels intestinal inflammation. But here is the data that matters:
Clinical Remission Rate at 1 Year (Crohn’s)
According to Eli Lilly’s FDA Approval Data (Jan 2025), in the Phase 3 VIVID-1 trial, 53% of Crohn’s patients achieved clinical remission at one year compared to just 36% on placebo. But it gets better.
The “deep healing” stats are what impress gastroenterologists. Data from the VIVID-1 Clinical Trial Results (2024) shows that Mirikizumab users saw a 46% rate of visible intestinal healing (endoscopic response) at one year, nearly double the placebo group.
Who is this for? This is becoming a top-tier option for patients who struggle specifically with bowel urgency and have failed older biologics like Humira or Remicade.
2. Upadacitinib (Rinvoq): The Oral Game-Changer
Not everyone wants an infusion. Needles, scheduling, sitting in a chair for hours—it adds up. Upadacitinib is a daily pill, a JAK inhibitor that works fast. How fast? We are talking weeks, not months.
Real-world data published in Clinical Gastroenterology and Hepatology (March 2025) indicates that 52.1% of patients achieved clinical remission within just 12 weeks of starting Upadacitinib.
This speed is critical for someone in a severe flare who needs relief immediately but wants to avoid long-term steroids. Furthermore, if you are “bio-naive” (meaning you haven’t taken biologics before), the success rate is astronomical. A Multi-Centre Real-World Study (2025) found that for bio-naive patients, Upadacitinib achieved a stunning 97.7% clinical remission rate at 6 months.
3. Stem Cell Therapy: Healing the Unhealable
For years, perianal fistulas have been the nightmare of Crohn’s disease—painful tunnels that often refuse to heal with standard drugs or surgery. Enter Mesenchymal Stem Cells (MSCs).
This isn’t science fiction anymore. Doctors are injecting stem cells directly into the fistula tract. These cells don’t just “patch” the hole; they modulate the immune system locally to encourage tissue regeneration.
According to a comprehensive umbrella review published by the NIH/PubMed (Dec 2024), stem cell therapy increased the likelihood of fistula healing by 48.1% compared to standard care. That is nearly a coin flip of success for a condition that previously had very low cure rates.
4. Bioelectronic Medicine: Vagus Nerve Stimulation (VNS)
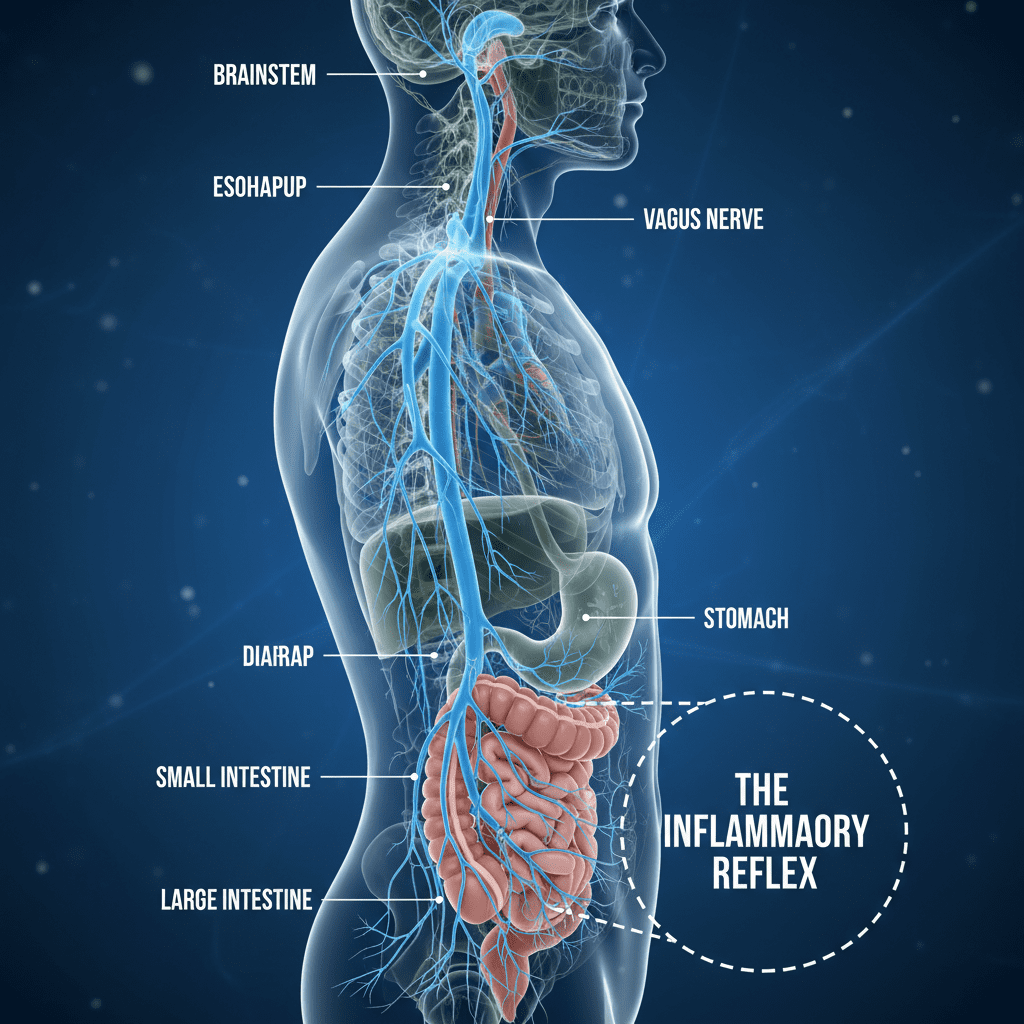
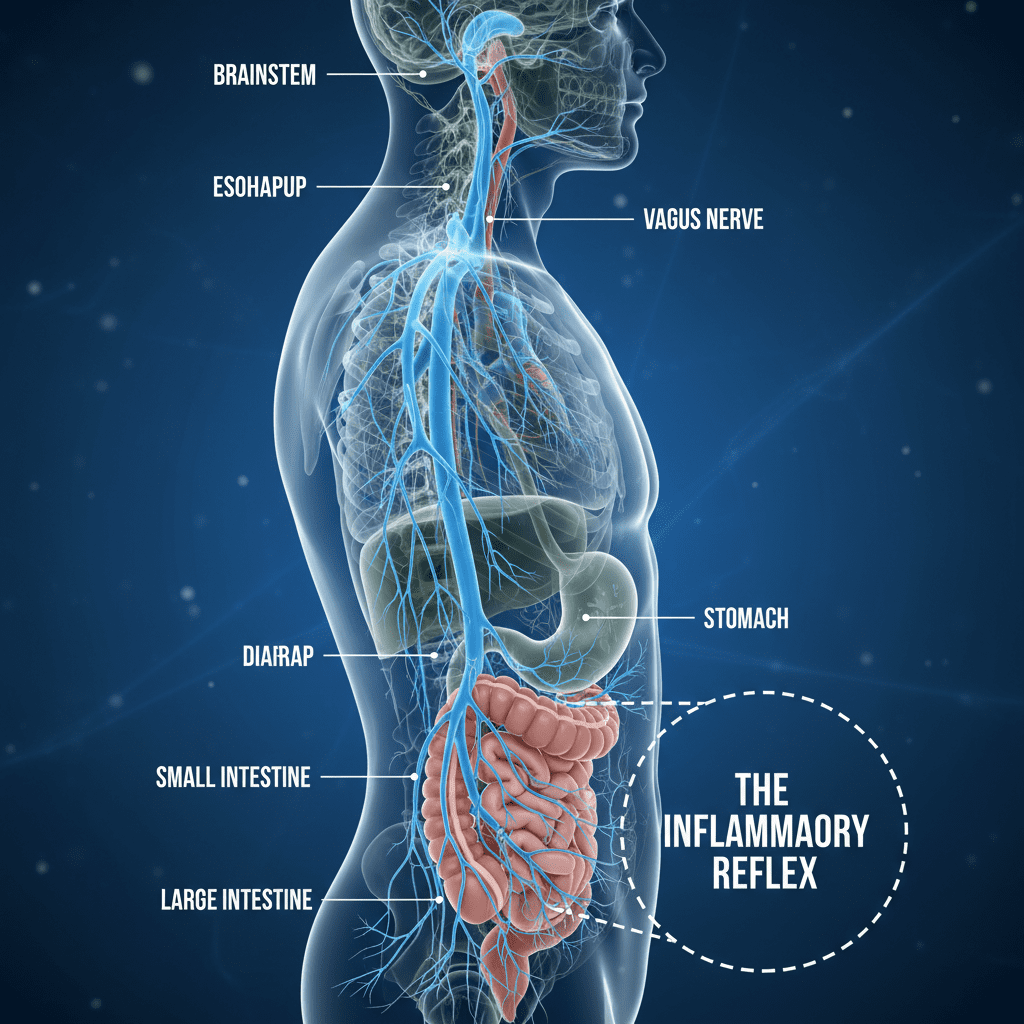
Here is where things get fascinating. We know the gut and brain are connected via the Vagus Nerve. This nerve acts as a superhighway for information. The “Inflammatory Reflex” theory suggests that if the Vagus Nerve is underactive, inflammation runs wild. Conversely, stimulating it can hit the brakes on the immune system.
New, non-invasive ear devices (which look like earbuds) deliver electrical pulses to the auricular branch of the Vagus Nerve. A groundbreaking study from the Feinstein Institutes for Medical Research (2024) showed that non-invasive VNS led to 50% remission in Crohn’s patients and a 50% reduction in fecal calprotectin levels (a key marker of inflammation).
This is drug-free, side-effect-free, and represents the frontier of “Bioelectronic Medicine.”
5. Etrasimod (Velsipity): The Immune Traffic Controller
Think of your lymphocytes (white blood cells) as soldiers. In Ulcerative Colitis, too many soldiers are rushing into the gut, causing damage. Etrasimod is an S1P receptor modulator. Essentially, it acts as a traffic controller, telling those lymphocytes to stay in the lymph nodes rather than attacking the colon.
It’s another oral option (pill) approved recently. It’s particularly exciting because of its safety profile and its ability to maintain remission without the risk of developing antibodies, which is a common failure point for traditional biologics.
The “Daily Defense”: 5 Lifestyle Hacks Backed by Science
Medication puts out the fire, but lifestyle prevents the sparks. However, we aren’t talking about generic “eat your veggies” advice. We need protocols backed by clinical data.
1. The CDED Strategy (Crohn’s Disease Exclusion Diet)
Diet is controversial in IBD, but the Crohn’s Disease Exclusion Diet (CDED) is changing the conversation. This isn’t just about eating healthy; it’s a structured exclusion of specific emulsifiers, animal fats, and additives that disrupt the microbiome.
The stats are undeniable. According to an MDPI Systematic Review (2024), in rapid responders, the CDED achieved a 75.4% remission rate by week 6. It works by starving the “bad” bacteria that thrive on processed foods and feeding the mucosal lining.
2. Gut-Directed Hypnotherapy
I know what you’re thinking. Hypnosis? Really? But remember the brain-gut axis we discussed earlier.
Stress signals from the brain can physically increase intestinal permeability (leaky gut). Gut-directed hypnotherapy breaks this cycle. A study from Northwestern University (Aug 2025) found that gut-directed hypnotherapy helped 68% of UC patients maintain remission for one year, compared to only 40% in the control group.
This suggests that managing the nervous system is just as important as managing the immune system.
3. Circadian Synchronization (The “Social Jet Lag” Factor)
Your gut bacteria have a clock. Seriously. When you sleep erratically, you disrupt the circadian rhythm of your microbiome, leading to spikes in inflammatory cytokines like IL-6.
The hack? strict sleep/wake times. Going to bed and waking up at the same time every day—even on weekends—can lower baseline inflammation levels.
4. Time-Restricted Eating (Mucosal “Rest” Periods)
When you are constantly digesting, your gut lining never gets a break to repair itself. This repair process is called autophagy—the body’s way of cleaning out damaged cells.
Implementing a 12-14 hour fasting window (e.g., stop eating at 7 PM, eat breakfast at 9 AM) allows mucosal healing to occur. While extreme fasting can be dangerous for malnourished IBD patients, this moderate “Time-Restricted Eating” supports the natural repair cycle without risking calorie deficiency.
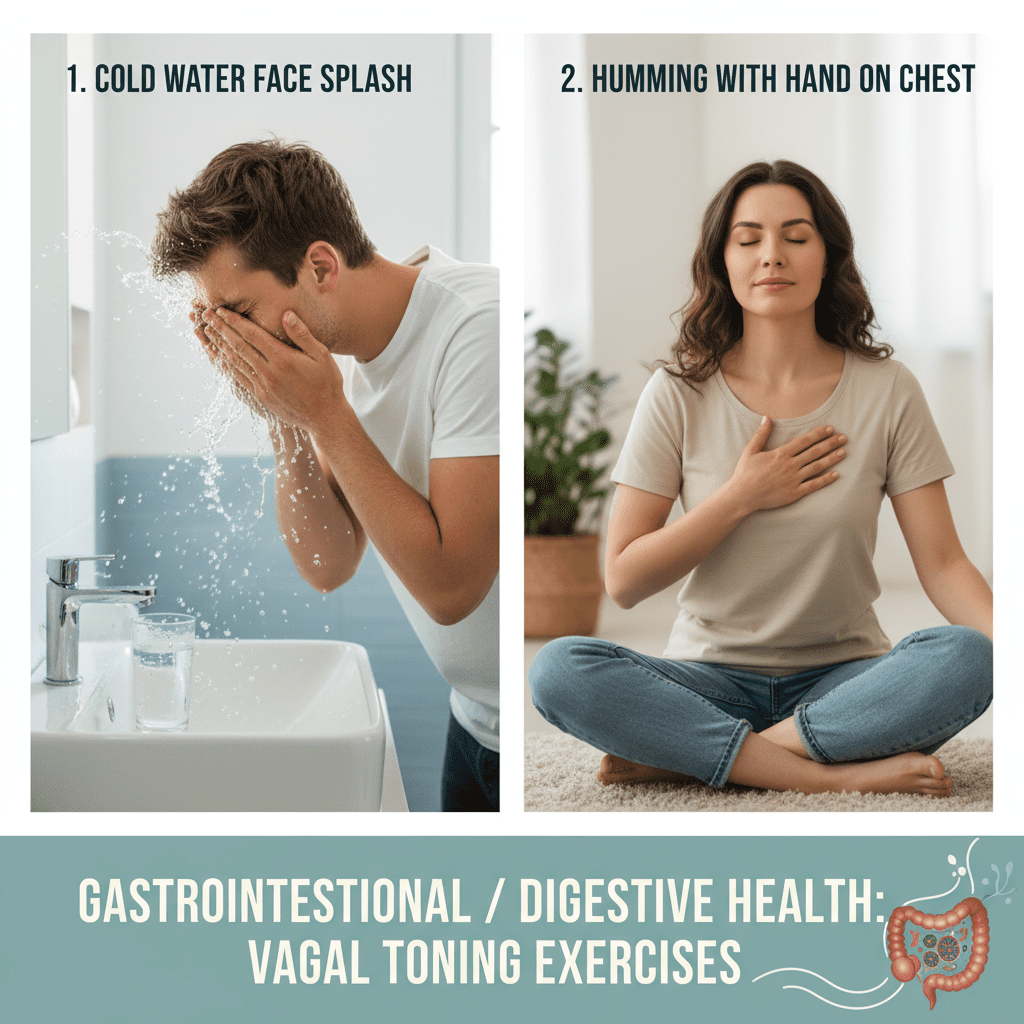
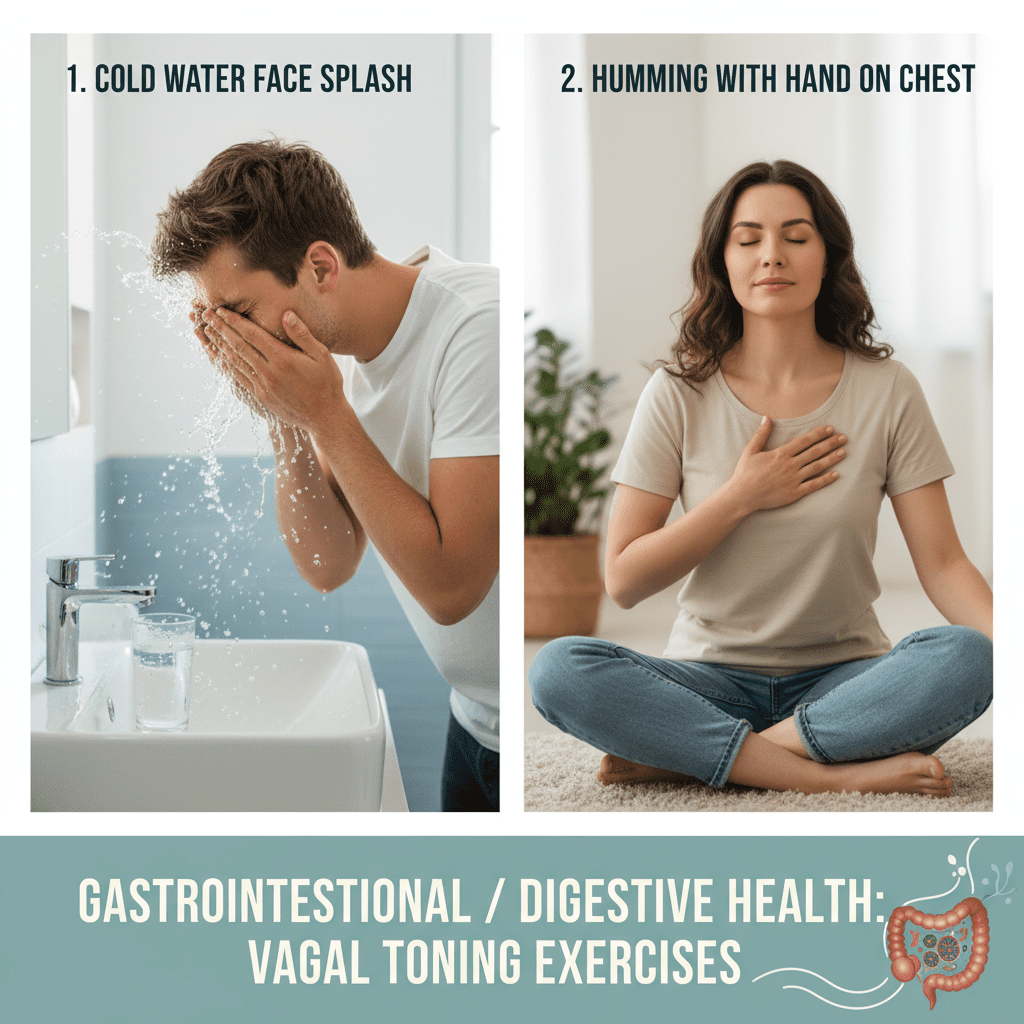
5. DIY Vagal Toning
If you can’t access a VNS device yet, you can stimulate the Vagus Nerve manually. The nerve passes through the vocal cords and the neck muscles.
- Humming or Chanting: The vibration stimulates the nerve endings. Five minutes of deep humming a day can lower heart rate and engage the parasympathetic nervous system.
- Cold Exposure: Splashing freezing water on your face stimulates the “diving reflex,” which is mediated by the Vagus Nerve.
Remission Rates Comparison: What the Data Says
To give you a clearer picture, here is how these new treatments stack up against each other based on the 2024-2025 data we’ve reviewed.
Clinical Remission Rates (Snapshot)
*Percentages based on specific study parameters cited in this article. “Bio-Naive” refers to patients who have never taken biologics.
Frequently Asked Questions (FAQ)
Is Mirikizumab approved for Crohn’s disease in 2025?
Yes. Based on the VIVID-1 trial results and subsequent regulatory actions, Mirikizumab (Omvoh) is positioned as a key therapy for Crohn’s disease in 2025, specifically targeting IL-23 to reduce bowel urgency and promote mucosal healing.
Can diet alone cure Crohn’s disease?
While “cure” is a strong word, diet can induce remission. The CDED (Crohn’s Disease Exclusion Diet) has shown remission rates as high as 75.4% in rapid responders according to 2024 reviews. However, for moderate to severe cases, it is often used in conjunction with medication.
What is the newest drug for Ulcerative Colitis in 2025?
Etrasimod (Velsipity) and Mirikizumab (Omvoh) are among the newest heavy hitters. Etrasimod offers an oral pill option that prevents immune cells from entering the gut, while Mirikizumab is an injectable biologic targeting specific inflammatory proteins.
Does intermittent fasting help IBD inflammation?
Yes, specifically through a mechanism called autophagy. By practicing Time-Restricted Eating (e.g., 12-14 hour fasting windows), you allow the gut mucosa a period of rest and repair, which can help lower inflammatory markers.
The Future is Personalized
If there is one takeaway from the research emerging in 2025, it is this: You have options. The days of simply accepting a life of pain and urgency are ending.
Whether it is the rapid action of oral JAK inhibitors like Upadacitinib, the deep mucosal healing of Mirikizumab, or the drug-free approach of Vagus Nerve Stimulation, the toolkit for fighting IBD has never been fuller.
But knowledge is only potential power. Real power comes from action. I encourage you to take these statistics—specifically the remission rates and mucosal healing data—to your next gastroenterology appointment. Ask about your eligibility for these newer therapies. Discuss the CDED diet. Advocate for your quality of life.
The inflammation can be reversed. The gut can heal. And in 2025, the odds of achieving that are finally stacking in your favor.