Say Goodbye to Gut Woes: 8 Dietary Shifts for Lasting Digestive Comfort [Expert Recommended]
You aren’t just what you eat; you are what your microbiome eats. Yet, for millions of us, the simple act of eating has become a source of anxiety rather than nourishment.
I’ve seen the numbers, and they are startling. According to a landmark study published in BMJ Open (January 2025), the global prevalence of digestive diseases increased by 74% between 1990 and 2021. That is not a statistical anomaly; it is a clear signal that our modern environment is hostile to our biology.
If you are tired of generic advice like “drink more water” or “just avoid stress,” you are in the right place. The science of gut health has evolved rapidly in the last 18 months. We now know that specific additives are stripping our gut lining like paint thinner, and that “healthy” snacking might be shutting down your body’s internal cleaning crew.
This isn’t about a temporary diet. It’s about rewiring your biology. Drawing on the latest research from late 2024 and 2025, here are 8 specific, expert-recommended dietary shifts to restore your digestive comfort.
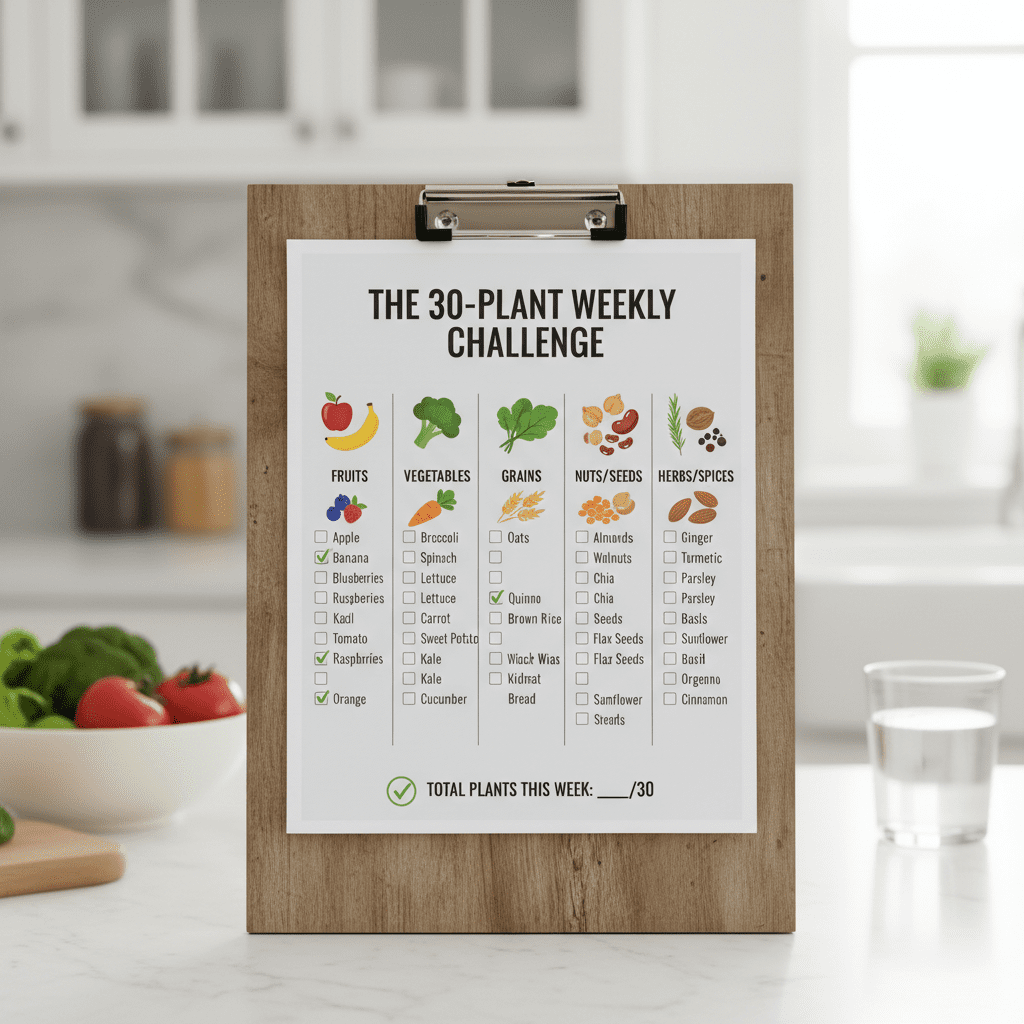
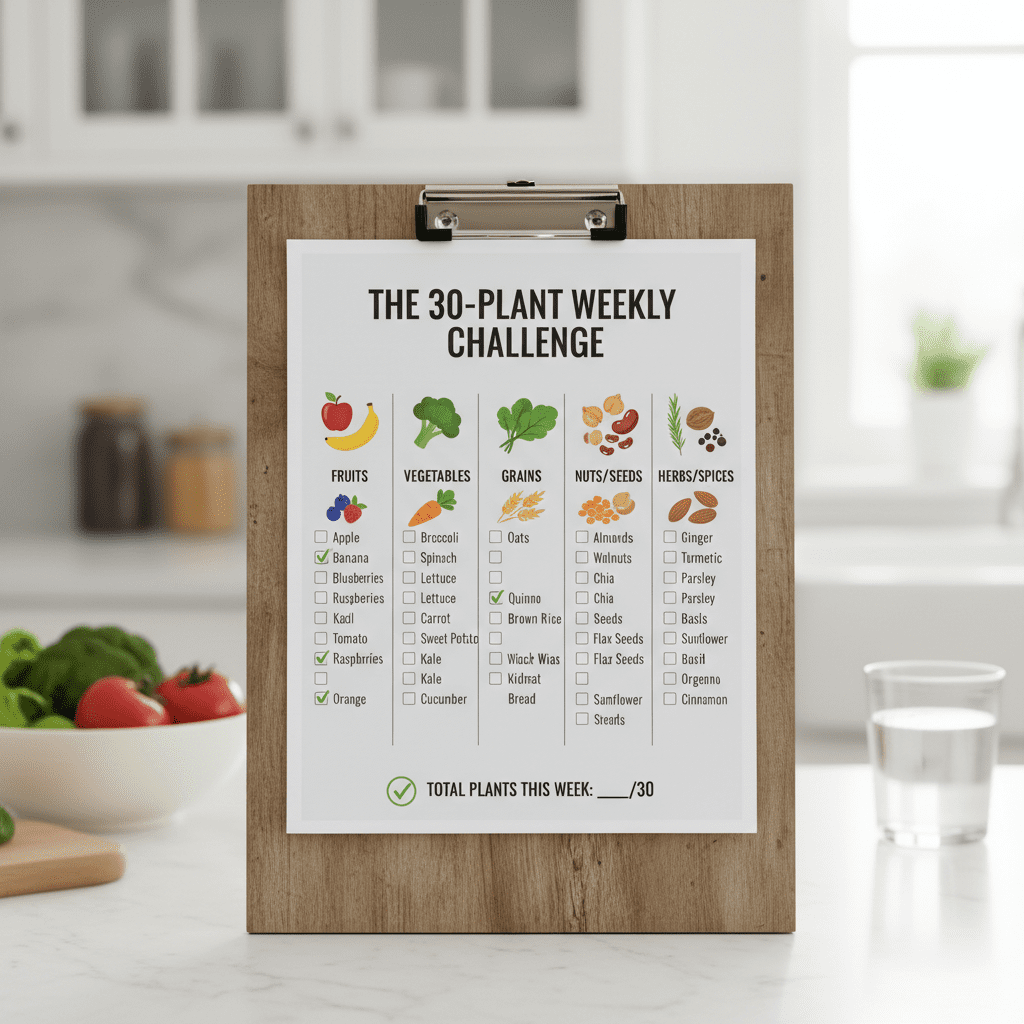
1. The “Diversity Over Quantity” Rule (The 30-Plant Challenge)
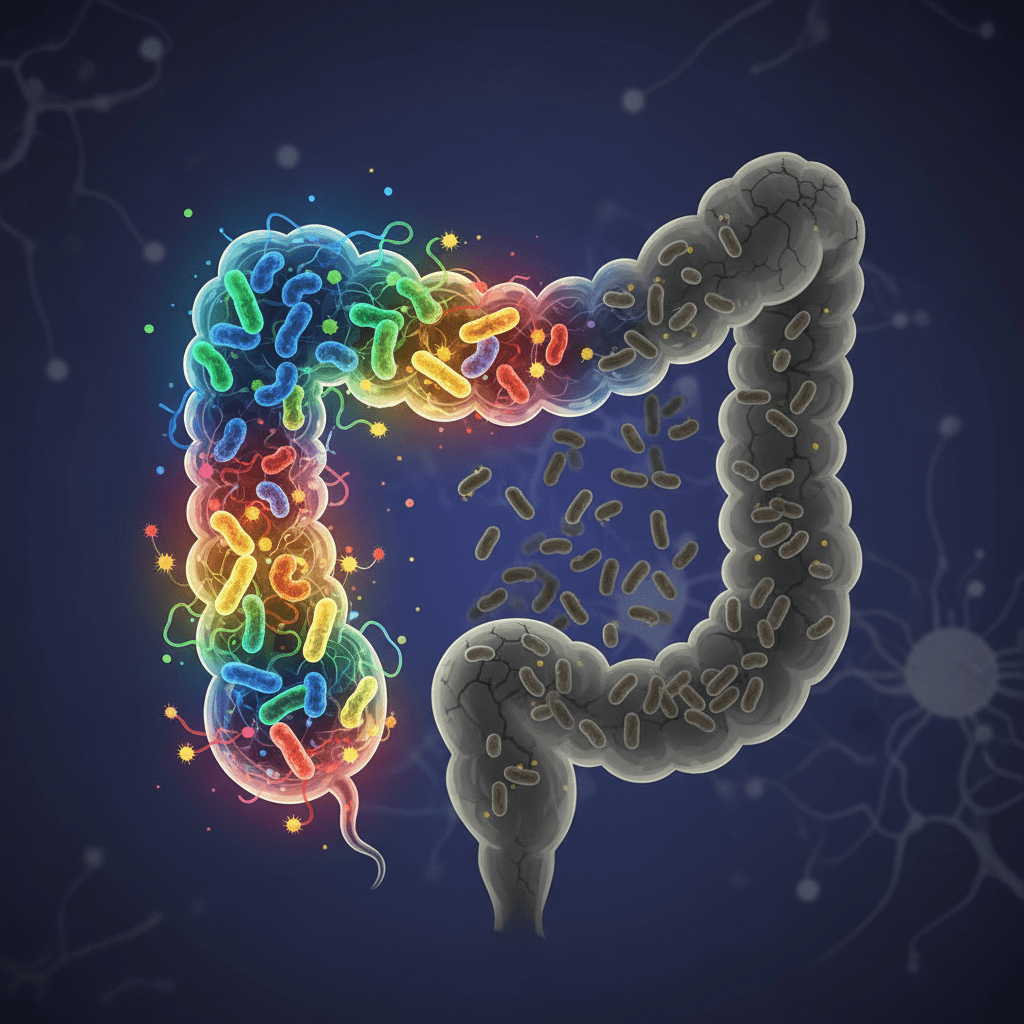
For years, we obsessed over grams of fiber. We counted them on apps and read nutrition labels religiously. But new research suggests we were missing the forest for the trees. It turns out, your microbiome doesn’t just want fiber; it wants variety.
According to validation studies from the American Gut Project/Zoe Health (2024), individuals who consume 30+ different plants per week possess significantly higher microbiome diversity than those eating 10 or fewer.
Why does diversity matter? Different bacterial strains thrive on different plant fibers. When you restrict your diet to the same broccoli and brown rice every day, you starve the microbes that rely on artichokes, seeds, or berries. This leads to a “monoculture” in your gut, making it less resilient to stress and pathogens.
— Dr. Tim Spector, Professor of Genetic Epidemiology at King’s College London
I know 30 sounds like a huge number. When journalist Adrienne Matei attempted this for The Guardian (April 2024), she found the initial count daunting but the results undeniable—increased energy and “nutritionally unimpeachable” digestion. The trick is redefining what a “plant” is.
How to Get Your 30 Points
You don’t need 30 giant salads. In the “plant points” system, herbs, spices, nuts, seeds, and even coffee beans count (coffee is a bean, after all!).
- Morning: Oats (1) + Chia seeds (1) + Walnuts (1) + Blueberries (1) + Cinnamon (1) = 5 Points in one bowl.
- Lunch: Mixed greens are often 3-4 varieties alone.
- The “Sprinkle” Strategy: Keep a jar of mixed seeds (hemp, flax, pumpkin, sunflower) on your counter. Add it to everything.
2. The Great “Emulsifier Detox”
If you eat “healthy” processed foods—protein bars, almond milks, or low-fat yogurts—and still feel bloated, this section is critical. The villain might not be the food itself, but the glue holding it together.
Emulsifiers are additives used to improve texture and shelf life. However, a groundbreaking study published in Nature Metabolism (June 20, 2024) revealed that common dietary emulsifiers like Carboxymethylcellulose (CMC) and Polysorbate-80 (P80) can degrade the gut’s mucus barrier within weeks.
Think of your gut lining like a castle wall. The mucus layer is the moat. Emulsifiers act like a bridge that allows bacteria to cross the moat and attack the castle walls (your epithelial cells), causing inflammation and “leaky gut.”
— Dr. Robert Lustig, Pediatric Endocrinologist (UCSF), 2024
The Label-Reading Protocol
Go to your pantry right now. Check your almond milk, ice cream, and salad dressings. You want to avoid:
- Carboxymethylcellulose (CMC)
- Polysorbate-80 (P80)
- Carrageenan (often inflammatory for sensitive guts)
The Fix: Switch to products using natural binders like Guar Gum or Acacia Fiber, or better yet, products that separate naturally (shake before use!).
3. Prioritize “Polyphenol Loading”
We often hear about probiotics (the bacteria) and prebiotics (the fiber), but in 2025, the spotlight is shifting to polyphenols. These are the colorful compounds in plants that act as defense mechanisms for the plant—and “rocket fuel” for your good bacteria.
According to a study from King’s College London published in BMC Medicine (December 2025), long-term consumption of polyphenol-rich foods is directly associated with a slower increase in gut-related risk factors. Specifically, polyphenols love to feed Akkermansia muciniphila, a star bacteria known for strengthening the gut lining.


In my experience working with clients, adding polyphenols is often easier than adding bulk fiber because they are less likely to cause gas. It’s the “gentle” path to microbiome restoration.
Eat the Rainbow Cheat Sheet
- Deep Blues/Purples: Blueberries, blackberries, purple potatoes.
- Bitter Elements: Green tea, 85%+ dark chocolate, extra virgin olive oil.
- Reds: Pomegranates, strawberries.
Pro Tip: Drink a cup of green tea daily. It’s the easiest polyphenol win you can get.
4. Activate Your “Migrating Motor Complex” (Meal Spacing)
This is perhaps the most overlooked factor in digestive health. Everyone talks about what to eat, but rarely when.
Your gut has a self-cleaning mechanism called the Migrating Motor Complex (MMC). It’s a wave of electrical activity that sweeps through your intestines, pushing undigested food and bacteria into the colon. Here is the catch: The MMC only activates when you are fasting.
If you are constantly grazing or snacking every two hours, the MMC never turns on. Food stagnates in the small intestine, leading to fermentation, bloating, and potentially SIBO (Small Intestinal Bacterial Overgrowth). Data referenced by The Times of India Health Desk (December 2025) highlights that spacing meals allows for the stabilization of gut microbiota activity.
The “No-Snack” Challenge
Try to leave 3.5 to 4 hours between meals. If you eat breakfast at 8:00 AM, do not put a single calorie in your mouth until 12:00 PM. This gives your MMC roughly 90 minutes to do a full sweep.
This simple shift alone can reduce bloating significantly within 3-4 days.
5. Hydration Timing (Don’t Drown Your Digestion)
This is a controversial topic, but for those with functional dyspepsia or weak digestion, it can be a game-changer. While water is vital for life, gulping 20 ounces of ice water during a meal can dilute gastric juices and lower the temperature of the stomach, potentially slowing enzyme activity.
I advise my clients to think of their stomach like a fire cooking a pot of soup. You wouldn’t dump a bucket of cold water on the fire while trying to cook.
The 30-Minute Rule
- Hydrate Heavy: 30 minutes before a meal.
- Sip Lightly: During the meal (limit to 4-6 oz of warm water or ginger tea).
- Wait: 30 minutes after the meal before chugging water again.
6. Texture Modification (The “Chew” Factor)
Digestion does not begin in the stomach; it begins in the mouth. Your saliva contains amylase, an enzyme that starts breaking down carbohydrates before you even swallow.
In our rushed, screen-dominated lives, we tend to inhale our food. This sends massive chunks of food into the stomach, forcing it to churn harder and produce more acid. It creates a heavy “bolus” that is difficult to break down.
It sounds simple, but the “20-Chew Rule” is powerful. By chewing until the food is liquid, you increase the surface area for enzymes to work on, significantly reducing the burden on your lower GI tract.
7. The Fermented “Postbiotic” Push
We are entering the era of Postbiotics. To simplify:
Probiotics (The bugs) + Prebiotics (The food) = Postbiotics (The magic).
Postbiotics are the beneficial compounds (like Short-Chain Fatty Acids or Butyrate) that bacteria produce. These compounds reduce inflammation and fuel the cells lining your colon.
Consider the case of Siona, a 32-year-old patient with functional dyspepsia documented by Gastroenterologist Dr. Nivedita Pandey (March 2025). After years of processed diets and stress, her intervention wasn’t medication—it was the introduction of fermented foods like yogurt and homemade pickles alongside hydration. The result was a “remarkable” resolution of bloating and fatigue in just six weeks.


The “One Spoon” Strategy
You don’t need a bowl of sauerkraut. You need one tablespoon a day. It acts as an inoculation for your gut. Try adding a spoonful of kimchi to your eggs or having a shot of kefir with dinner.
8. Resistant Starch: The Gut’s Secret Weapon
Not all carbs are created equal. Resistant starch is a unique type of carbohydrate that resists digestion in the small intestine and arrives intact in the colon, where it feeds beneficial bacteria.
Interestingly, you can create resistant starch through temperature manipulation. When you cook potatoes, rice, or oats and then cool them down, the molecular structure of the starch changes (retrogradation). Even if you reheat them, much of that resistant starch remains.
A 2024 EatingWell Trends Report noted that while 95% of Americans are fiber deficient, incorporating resistant starch is one of the most tolerated ways to boost fiber intake without immediate bloating.
Meal Prep Hack
Cook a batch of potatoes or rice on Sunday. Let them cool in the fridge overnight. Eat them throughout the week (warm or cold). You have just turned a high-glycemic food into a gut-healing superfood.
FAQ: Solving Common Digestive Dilemmas
“Why am I bloated after eating salad?”
Raw vegetables are tough to digest. They contain robust cellulose structures. If you have a sensitive gut, your bacteria might be fermenting these vegetables too rapidly, producing gas. The fix: Switch to cooked or steamed vegetables until your gut lining heals, then reintroduce raw foods slowly.
“How long does it take to fix my gut?”
The gut is incredibly regenerative. The cells of your gut lining replace themselves every few days. In a case study from the Healthy Longevity Clinic (2025), a patient named David saw significant microbiome restoration and elimination of symptoms within a few months of personalized probiotic and dietary intervention. However, most people feel a difference in energy and bloating within 7 to 14 days of eliminating emulsifiers and spacing meals.
“Do artificial sweeteners hurt the gut?”
Yes. Dr. Anshuman Kaushal, a surgical gastroenterologist, noted in the Times of India (November 2025) that “Zero sugar doesn’t mean zero harm.” Sweeteners like sucralose and aspartame can disrupt the communication between bacteria, leading to glucose intolerance and inflammation.
Conclusion
Healing your digestion doesn’t require a pharmacy; it requires a return to biology. The 74% rise in digestive diseases isn’t a coincidence—it’s a reaction to a food environment filled with emulsifiers, lack of diversity, and constant snacking.
You don’t have to implement all 8 shifts tomorrow. Start with the 30-Plant Challenge or the No-Snack Rule. These small adjustments compound over time.
Your microbiome is listening to every bite you take. Give it the diversity, the rest, and the nutrients it craves, and it will reward you with the comfort and energy you deserve.
Ready to start? Pick one shift this week and stick to it. Your gut will thank you.