Banish Bloating & IBS: 7 Proven Strategies for Fast Relief [2025 Expert Guide]
You know the feeling. You wake up with a flat stomach, eat a seemingly harmless lunch—maybe just a salad—and by 3:00 PM, you look six months pregnant. Your pants are digging into your waist, the pressure is mounting, and you just want to unbutton everything and lie down.
In my years of consulting with digestive health clients, the “IBS Bloat” is the single most frustrating symptom I encounter. It destroys body image, ruins social plans, and creates a cycle of anxiety around food. But here is the thing that most generic health websites won’t tell you: drinking more water and eating more fiber might actually be making you worse.
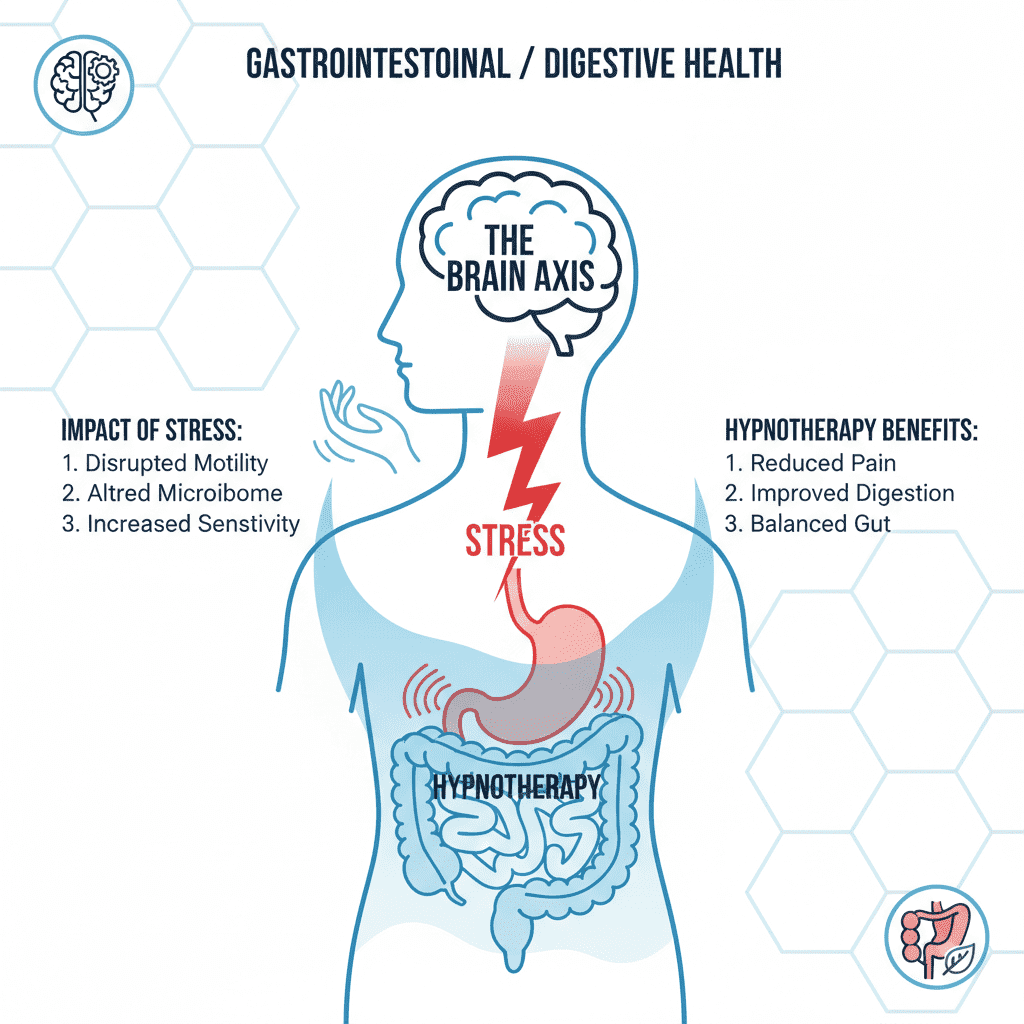
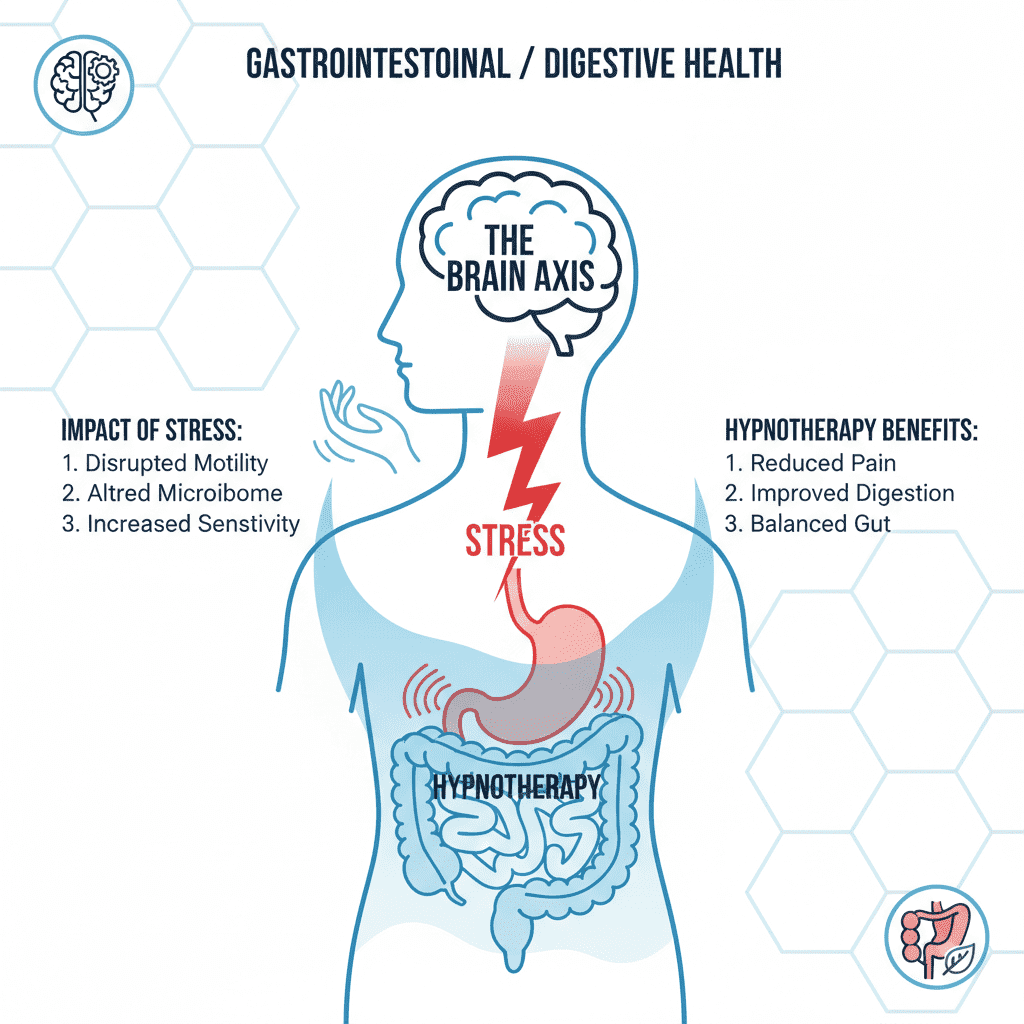
The landscape of IBS treatment has shifted dramatically in the last 12 months. We are no longer just guessing at triggers. New data from 2024 and 2025 has highlighted the incredible power of the brain-gut axis and specific enzyme therapies over restrictive dieting.
This isn’t just another list of home remedies. This is a science-backed protocol based on the latest research from Monash University and the University of Gothenburg, designed to stop the bloat now and prevent it from coming back.


In This Article:
- The Science: Why You Look Pregnant (It’s Not Just Gas)
- Strategy 1: The “Emergency Flush” Protocol
- Strategy 2: Targeted Movement for Entrapment
- Strategy 3: The Modified Low-FODMAP Diet (2025 Update)
- Strategy 4: Gut-Directed Hypnotherapy
- Strategy 5: Smart Supplementation
- Strategy 6: Hydration & The Tea Fix
- Strategy 7: When to See a Doctor
The Science of the “IBS Belly”: Why You Bloat
To fix the problem, we have to understand the mechanism. Most people assume bloating is simply an accumulation of gas. While gas plays a role, for IBS sufferers, the issue is often Visceral Hypersensitivity.
Imagine your gut has a volume knob. For most people, that knob is set to 3. They digest food, gas is produced, and they don’t feel it. If you have IBS, your volume knob is stuck at 10. Normal digestion feels like a crisis. Your abdominal muscles may even relax and protrude in response to this sensation—a condition known as abdomino-phrenic dyssynergia. You aren’t just imagining the distension; your body is physically reacting to a false alarm.
of the global population suffers from IBS, with women (14.0%) significantly more affected than men.
According to Buoy Health / Meta-Analysis, Oct 2024.
However, we must also rule out the imposters. In some cases, what looks like IBS is actually Small Intestinal Bacterial Overgrowth (SIBO). This occurs when bacteria migrate from the colon up into the small intestine, where they ferment food prematurely. If you bloat within 30-60 minutes of eating, SIBO is a prime suspect. But assuming it’s classic IBS, let’s look at how to stop the pain immediately.
Strategy 1: The “Emergency Flush” Protocol (Immediate Relief)
You’re in pain right now? Forget the long-term diet changes for a moment. You need to de-escalate the situation. Here is the “Emergency Flush” protocol I recommend for acute flare-ups.
1. Enteric-Coated Peppermint Oil
This is nature’s calcium channel blocker. It relaxes the smooth muscles of the intestines, preventing the spasms that trap gas. The “enteric-coated” part is non-negotiable—if the capsule dissolves in your stomach, you’ll just get heartburn. It needs to reach the intestines.
2. Simethicone + Heat
Combine a standard dose of Simethicone (Gas-X) with a hot water bottle or heating pad placed directly on the lower abdomen. The Simethicone breaks large gas bubbles into smaller ones that are easier to pass, while the heat increases blood flow and relaxes the cramping muscles. It’s a simple combo, but in my experience, it works faster than almost anything else.


Strategy 2: Targeted Movement for Gas Entrapment
When gas is trapped, sitting on the couch is the worst thing you can do. You need to physically manipulate the colon to move the gas toward the exit. I’m not talking about a HIIT workout—intense cardio can actually shut down digestion (fight or flight response). We want gentle compression.
The “Wind-Relieving” Pose (Pawanmuktasana)
This yoga staple is named literally for what it does. Lying on your back, hug your knees to your chest. Rock gently side to side. This compresses the ascending and descending colon, manually massaging the gas through.
The 15-Minute Rule
Make a pact with yourself: After every meal, you walk for 15 minutes. Not a run, just a walk. This stimulates gastric emptying. If food sits in your stomach too long, it ferments. Walking pushes it along.
Strategy 3: The Modified Low-FODMAP Diet (The 2025 Approach)
For years, the Low-FODMAP diet has been the standard. It involves cutting out Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols. Essentially, carbohydrates that ferment poorly.
But here is the shift we are seeing in 2025: Strict elimination is causing “food fear.” Patients become afraid to eat anything. The modern approach is “Gentle FODMAP.” Instead of cutting everything, we just swap the highest offenders.
According to Dr. Chey’s updated data, two-thirds of IBS patients report symptoms triggered specifically by carbohydrates. Here is a quick swap guide to lower your load without starving yourself:
| High FODMAP (The Bloaters) | Low FODMAP (The Safe Bets) |
|---|---|
| Apples, Pears (High Fructose) | Kiwi, Blueberries, Oranges |
| Onion, Garlic (Fructans) | Garlic-infused Oil, Green Onion (Tops only) |
| Wheat Pasta | Quinoa, Rice Noodles, Sourdough Bread |
| Cow’s Milk | Lactose-Free Milk, Almond Milk |
And the science backs this dietary intervention over popping pills. A landmark study from the University of Gothenburg in April 2024 compared dietary treatment against medications. The result? 76% of patients had significantly reduced symptoms with diet versus only 58% in the medication group.
Strategy 4: Gut-Directed Hypnotherapy (The New Gold Standard)
If you take one thing away from this article, let it be this: Your gut and brain are talking, and right now, they are arguing.
Gut-Directed Hypnotherapy (GDH) is not “woo-woo” magic. It is a psychological therapy that rewires the communication between the brain and the gut to reduce visceral hypersensitivity. In 2025, this is becoming the preferred treatment for many gastroenterologists because it doesn’t require restrictive dieting.
of participants had a clinically significant decrease in abdominal pain using gut-directed hypnotherapy apps like Nerva.
According to Monash University / Nerva Trial, Oct 2024.
I’ve watched clients who failed every diet finally find relief through apps like Nerva. The premise is simple: calm the nervous system, and the gut stops overreacting to digestion. It turns that volume knob from a 10 back down to a 3.
Strategy 5: Smart Supplementation (Beyond Probiotics)
I am going to say something controversial: Stop taking random probiotics.
If you have SIBO or slow motility, throwing billions of bacteria into your system can actually increase fermentation and bloating. Unless you are using a specific strain proven for IBS (like *Bifidobacterium infantis* 35624), you might be adding fuel to the fire.
The Enzyme Alternative
Instead, look at digestive enzymes. specifically Alpha-galactosidase. This is the enzyme found in products like Beano. It helps break down the complex carbohydrates in beans, cruciferous vegetables, and grains before they hit the colon and ferment. It’s a proactive strike against gas.
Strategy 6: Hydration & The “Tea Fix”
We are told to drink water, but for IBS, how you drink matters. Chugging ice-cold carbonated water is a recipe for disaster. The carbonation introduces gas, and the cold temp can shock the stomach.
Switch to warm water or herbal teas. My go-to recommendation is Fennel Tea. Fennel acts as a carminative—it helps expel gas from the digestive tract. Ginger tea is another powerhouse, known for speeding up stomach emptying (motility) so food doesn’t sit and rot.
Strategy 7: Medical Interventions (When to See a Doctor)
Sometimes, lifestyle changes aren’t enough. According to the IFFGD (International Foundation for Gastrointestinal Disorders), IBS results in between 2.4 and 3.5 million annual physician visits in the US alone.
If you have tried the strategies above with no relief, you may need to discuss pharmacotherapy with a gastroenterologist. This might include:
- Rifaximin: A non-absorbable antibiotic often used to treat IBS-D and SIBO.
- Secretagogues: Medications like Linaclotide that increase fluid in the intestines to help with constipation (IBS-C).
- Low-dose Antidepressants: These are used not for depression, but to dampen the pain signals from the gut to the brain.
FAQ: Your Bloating Questions Answered by Experts
Does intermittent fasting help IBS bloating?
It can. By giving your gut a longer break (the Migrating Motor Complex), you allow it to “sweep” residual food and bacteria out of the small intestine. However, if fasting causes you to eat massive meals when you break the fast, it can backfire. Smaller, spaced-out meals are generally safer.
Can probiotics make IBS bloating worse?
Absolutely. As mentioned earlier, adding bacteria to an environment that might already have an overgrowth (SIBO) creates more fermentation. It’s often better to focus on removing triggers first, then rebuilding the microbiome later.
Is bloating a sign of ovarian cancer?
While bloating is a classic IBS symptom, persistent bloating that doesn’t go away (even overnight) can be a red flag. If you experience persistent bloating, pelvic pain, and feeling full quickly, consult a doctor immediately to rule out other conditions.
Conclusion: The “Banish Bloat” Action Plan
You do not have to live your life unbuttoning your pants under the dinner table. The “IBS belly” is complex, but it is manageable. Here is your summary for relief:
- Immediate: Use Peppermint Oil (enteric-coated) and heat for acute pain.
- Movement: Walk 15 minutes after meals and use the “Wind-Relieving” yoga pose.
- Diet: Adopt a “Gentle FODMAP” approach—swap the onions and garlic, but don’t starve yourself.
- Mind: Try Gut-Directed Hypnotherapy (Nerva) to fix the root cause in the brain.
Start with Strategy 1 for relief today, then begin Strategy 4 for lasting freedom. Your gut is listening—it’s time to change the conversation.
