Revitalize Your Inner Ecosystem: A Data-Backed Guide to Restoring Gut Microbiome
You’re eating yogurt, you’re taking a probiotic, but are you still bloated? You might be fighting the wrong war.
For years, I’ve watched clients obsess over counting fiber grams, yet their digestion remains a mess. The frustration is palpable, and frankly, heartbreaking. But new data has finally shed light on why generic advice fails.
A landmark 2024 study from the University of Cambridge reveals that 168 common household chemicals—not just your diet—might be silently killing your beneficial bacteria. This isn’t just about what you eat; it’s about what your environment is doing to you.
Forget the vague “eat healthy” platitudes. This guide cuts through the noise. By leveraging data from the new ‘Human Gut Microbiome Atlas’ and the latest clinical trials, we will walk through a precise, 3-step protocol on how to restore gut microbiome health effectively.
The Hidden War: Why Your Gut is Losing the Battle
Before we can rebuild, we have to understand the demolition crew. The medical term is “dysbiosis”—an imbalance where harmful bacteria outnumber the good. According to the International Microbiota Observatory’s 2024 Results, only 1 in 3 people worldwide even understand what dysbiosis is, despite it being a leading cause of chronic inflammation.
The consequences are severe. A global analysis published in EMJ Reviews in 2024 found that regions with high levels of gut dysbiosis are seeing an IBD (Inflammatory Bowel Disease) incidence rate 3.2 times higher than regions with balanced ecosystems.
The “Chemical Exposure” Study (Cambridge 2024)
Here is where the science has shifted dramatically. We used to think antibiotics were the only enemy. However, late 2024 research published in Nature Microbiology identified 168 common chemicals—including specific pesticides found on non-organic produce and plastic additives—that actively inhibit the growth of beneficial gut bacteria.
It turns out that non-antibiotic drugs and environmental toxins can be just as destructive.
“Our gut bacteria are likely coming into contact with many of the substances tested in the study… Safety testing must expand to consider gut health.”
— Dr. Kiran Patil, University of Cambridge (2024)
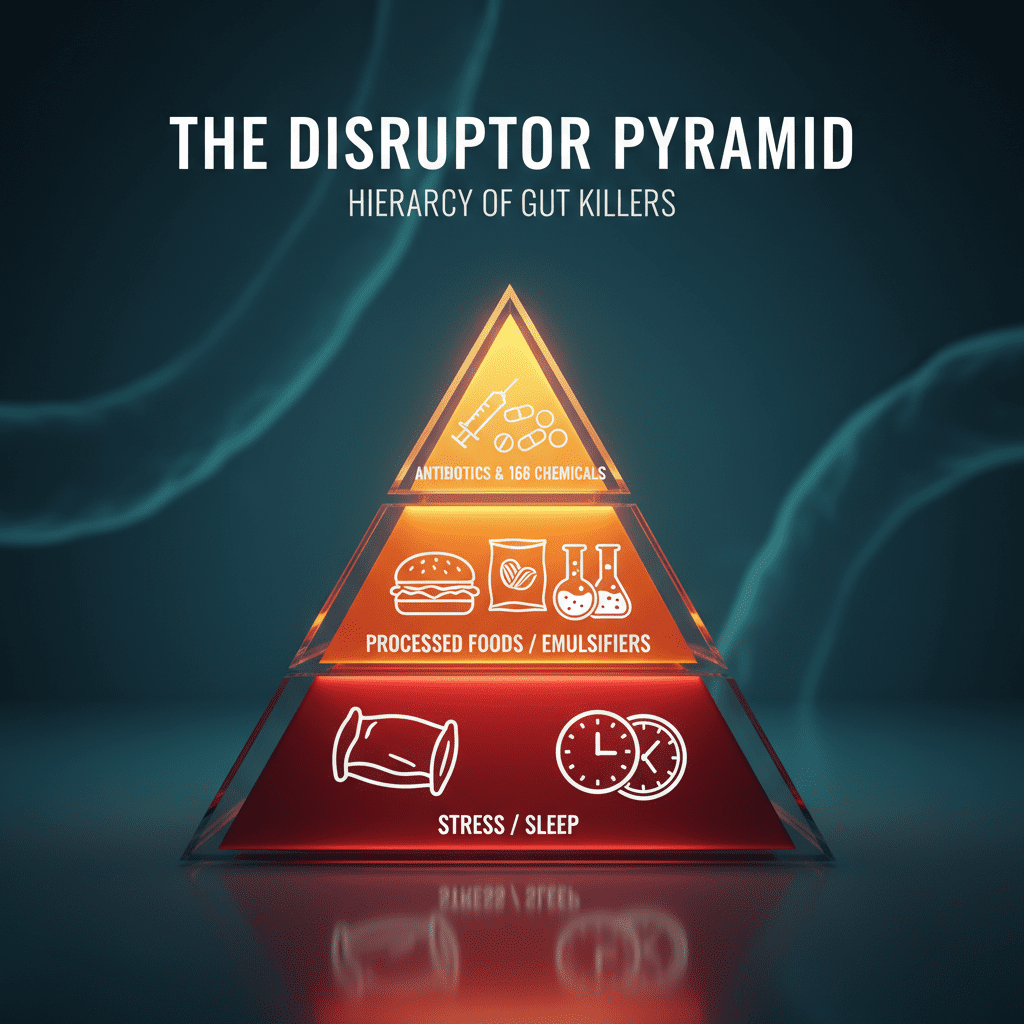
The Ultra-Processed Food Trap
It’s not just chemicals; it’s the structure of food itself. New data suggests that emulsifiers (chemicals used to keep packaged food smooth) act like detergents in the gut. They strip away the protective mucus layer, allowing bacteria to come into direct contact with the intestinal wall. This is the biological mechanism behind “leaky gut” or intestinal permeability.
When this barrier breaches, the immune system goes into overdrive. This explains why you might feel “brain fog” after a processed meal—your immune system is fighting a war in your gut that drains your energy.
Fermented Foods vs. Fiber: The Stanford Showdown
If you ask most people how to restore gut microbiome balance, they scream “FIBER!” But is fiber really the fastest way?
In a fascinating retrospective analysis released in 2024 by the Stanford School of Medicine, researchers pitted a high-fiber diet against a high-fermented-food diet. The results were shocking to many nutritionists.
Why Fiber Isn’t Enough (In the Short Term)
The study found that while high-fiber diets are crucial for long-term health, they often take longer than 10 weeks to significantly alter microbiome diversity in some adults. In fact, increasing fiber too quickly in a damaged gut can increase bloating because the bacteria required to digest that fiber aren’t there yet.
“We expected high fiber to have a more universally beneficial effect… but the data suggest that increased fiber intake alone over a short time period is insufficient to increase microbiota diversity compared to fermented foods.”
— Dr. Christopher Gardner, Stanford Prevention Research Center
The “6-Serving” Protocol
The winner was fermentation. The group consuming fermented foods showed increased diversity and decreased inflammatory markers in just weeks. The magic number? Six servings a day.
Now, before you panic, a “serving” isn’t a bowl. It’s small. Here is the Stanford-inspired cheat sheet:
- Kimchi or Sauerkraut: 1/2 cup (counts as 1 serving)
- Kefir or Yogurt: 1/2 cup (counts as 1 serving)
- Kombucha: 4-6 oz (counts as 1 serving)


The “Psychobiotic” Revolution: Gut Bacteria and Mental Health
Have you ever felt “butterflies” in your stomach when nervous? That is the enteric nervous system talking. We now know that 95% of your body’s serotonin is produced in the gut, not the brain. If your gut is inflamed, your mood crashes.
New AI Insights from King’s College
In July 2024, researchers at King’s College London utilized AI modeling within the Human Gut Microbiome Atlas project. They confirmed distinct microbiome signatures associated with depression. This validates the potential for “psychobiotics”—using bacteria to treat mental health.
Even more compelling is the “Twins Study” from King’s College (2024). They studied 36 pairs of twins over 60 years old. One twin took a cheap prebiotic (inulin/FOS), and the other a placebo. The result? The twin taking the prebiotic showed improved cognitive test scores and higher Bifidobacterium levels in just 12 weeks.
The takeaway: It is never too late to rebuild your gut-brain connection.
4-Step Protocol to Restore Balance (The “R.E.A.L.” Method)
Based on this 2025 research landscape, here is the R.E.A.L. method to rebuild your inner ecosystem.
R: Remove (The Chemical Detox)
You cannot heal a wound while you are still poking it. To address the Cambridge findings regarding the 168 disrupting chemicals:
- Filter Your Water: Chlorine is designed to kill bacteria in pipes; it does the same in your gut. Use a carbon block filter.
- Go Organic for the “Dirty Dozen”: Glyphosate acts as an antibiotic. If you can’t buy everything organic, prioritize thin-skinned produce (strawberries, spinach) and wheat products.
- Limit Artificial Sweeteners: Aspartame and sucralose have been shown to alter gut flora composition negatively.
E: Enrich (Fermentation First)
Follow the Stanford protocol. Aim for a gradual increase to 6 small servings of fermented foods daily. Start slow to avoid bloating—perhaps one tablespoon of sauerkraut with dinner, then scale up.
Pro Tip: Look for “Live Active Cultures” on labels. If the pickles are on a non-refrigerated shelf, they are likely vinegar-pickled and sterile (no bacteria).
A: Activate (Polyphenols & Fiber)
Once you have introduced the bacteria (via fermentation), you must feed them. This is where prebiotics come in. But don’t just eat fiber; eat color.
Polyphenols are the micronutrients that give food its color (like the dark blue in blueberries). They act as rocket fuel for Akkermansia muciniphila, a bacteria crucial for strengthening the gut lining. Eat berries, dark chocolate (85%+), and green tea.
L: Lifestyle (Circadian Syncing)
Your bacteria have a bedtime. Seriously. Research indicates that the microbiome has its own circadian rhythm. If you eat late at night, you disrupt the “Migrating Motor Complex” (MMC)—the cleaning wave that sweeps debris out of your small intestine.
Action: Fast for at least 12 hours overnight (e.g., finish dinner by 7 PM, breakfast at 7 AM) to let the MMC do its work.
Beyond Probiotics: The Rise of Postbiotics
You’ve heard of probiotics (the bugs) and prebiotics (the food). But the future of gut health, according to the 2024 Grand View Research market report, lies in Postbiotics.
Postbiotics are the waste products beneficial bacteria produce after they eat fiber. The most important one is Butyrate (a short-chain fatty acid). Butyrate is the primary fuel source for the cells lining your colon.
You can’t easily take postbiotics as a supplement because they degrade quickly. You must manufacture them internally. The best way to stimulate postbiotic production is consuming Resistant Starch—cooked and cooled potatoes, green bananas, or oats. These foods resist digestion in the stomach and arrive in the colon ready to be fermented into healing postbiotics.
FAQ: Your Gut Health Questions Answered
How long does it take to restore gut health?
Research from 2024 suggests diet changes alter bacteria in as little as 24-48 hours. However, restoring full diversity and healing the mucosal lining typically takes 10-12 weeks of consistent adherence to the R.E.A.L. protocol.
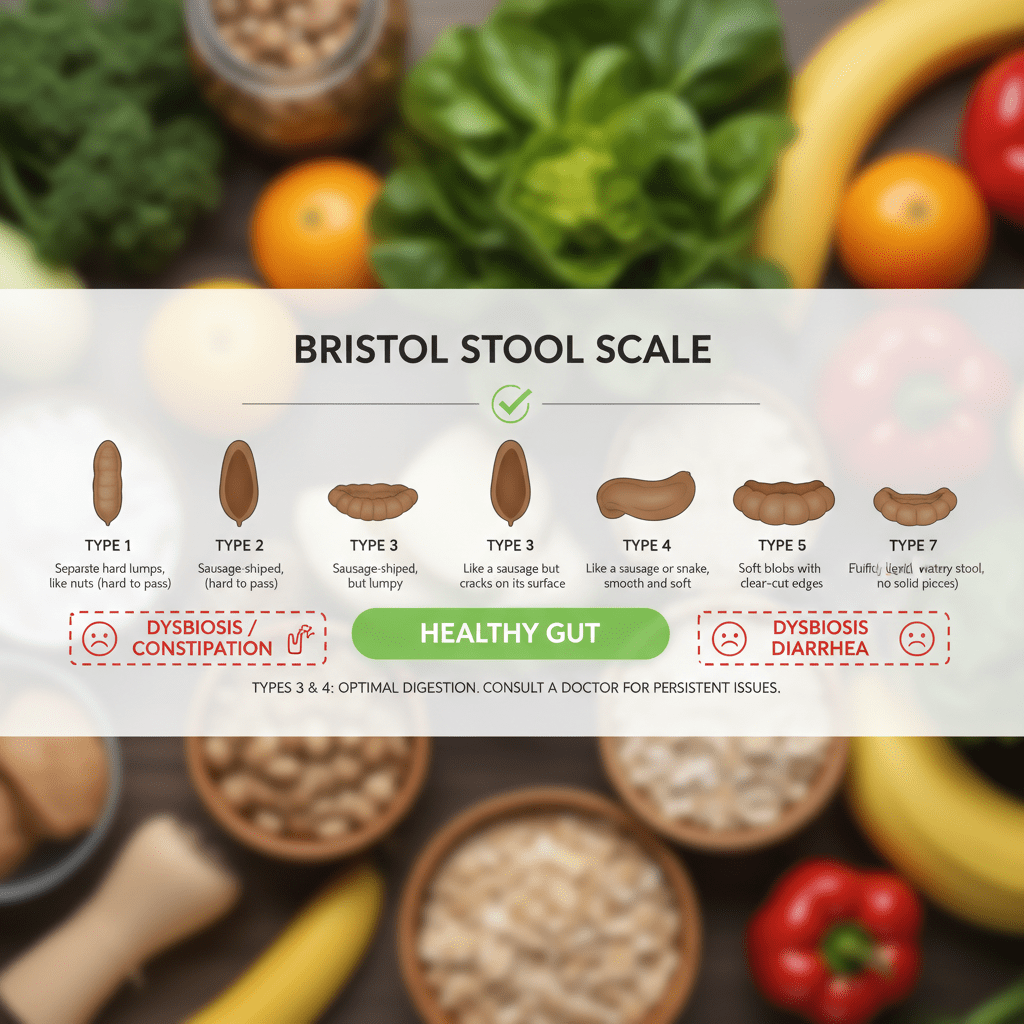
What are the signs that my gut is healing?
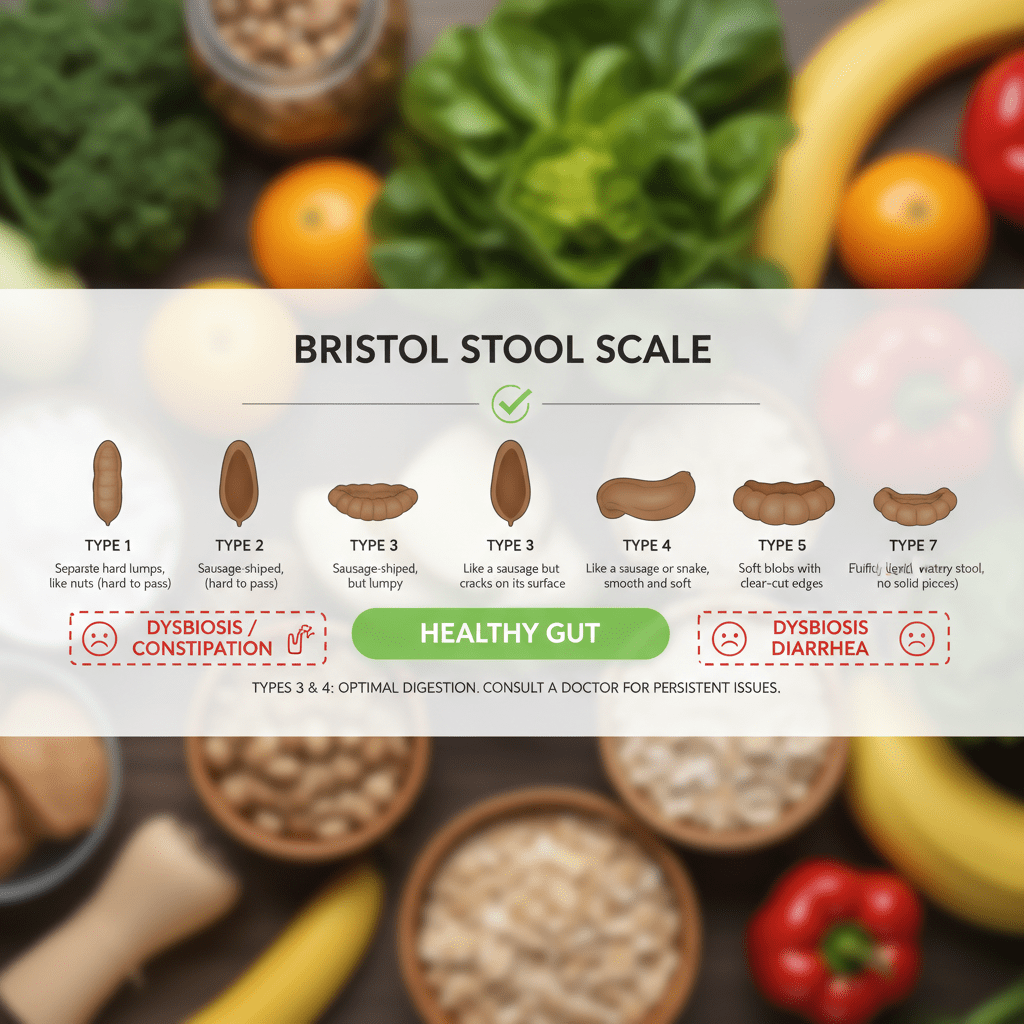
The first signs are usually reduced bloating after meals and more regular bowel movements (aiming for Bristol Scale type 3-4). Following that, many people report improved energy levels (“brain fog” lifting) and clearer skin within 3-4 weeks.
Does fasting reset the gut microbiome?
Yes. Intermittent fasting triggers the “Migrating Motor Complex” (MMC). This is a mechanical “sweeping” of the intestines that prevents bacterial overgrowth (SIBO) in the small intestine. A 12-16 hour overnight fast is ideal for this.
Can I heal my gut naturally without supplements?
Absolutely. The Stanford study proved that fermented foods were actually more effective at increasing diversity than fiber supplements in the short term. While specific probiotics (like spore-based strains) can help, whole foods should always be the foundation.
Does sugar really kill gut bacteria?
High sugar intake feeds pathogenic bacteria (like Candida) and suppresses beneficial strains like Bacteroides. It creates an environment where the “bad guys” can outcompete the “good guys,” leading to dysbiosis.
Final Thoughts: Start Small, Start Today
Restoring your gut microbiome isn’t about buying the most expensive supplement on the shelf. The science from Cambridge and Stanford points us toward a more fundamental truth: we must remove the environmental toxins inhibiting our flora and feed our inner ecosystem with living foods.
In my experience, the biggest mistake people make is trying to do everything at once. Don’t overhaul your entire life overnight. Start with the “Remove” phase—filter your water and check your food labels for emulsifiers. Then, add one scoop of sauerkraut to your dinner.
Your gut bacteria are resilient. Give them the right environment, and they will do the healing for you.