Silent Sufferers No More: 9 Hidden Digestive Conditions & How to Identify Them [Complete Checklist]
You’ve been told it’s “just IBS,” but the treatments aren’t working. You aren’t crazy—you might be misdiagnosed. Here is the definitive 2025 guide to what your doctor might be missing.
I’ve seen this happen time and time again. A patient walks in looking six months pregnant after eating a simple salad, only to be told to “reduce stress” and “eat more fiber.” It’s frustrating, it’s isolating, and frankly, it’s often medically inaccurate.
The reality is that “IBS” is a diagnosis of exclusion. It means “we know your gut isn’t working, but we don’t know why.” But medical science has advanced significantly in the last 24 months. What we used to call IBS is often a specific, identifiable, and—most importantly—treatable condition.
According to The Celiac Disease Foundation, a staggering 83% of Americans with celiac disease are undiagnosed or misdiagnosed with other conditions. That is just one condition. Imagine how many other “hidden” culprits are lurking behind that generic IBS label.
In this guide, we are going to peel back the layers. We will explore the 9 most common hidden digestive conditions that mimic IBS, backed by 2024 and 2025 research. I’ve also included a specific diagnostic checklist you can take to your next appointment.
The “Wastebasket Diagnosis”: Why Your Gut Issues Are Missed
Before we dive into the specific conditions, we need to understand the difference between a “functional” disorder and an “organic” disease. IBS is classified as a functional gastrointestinal disorder (FGID). This means the machinery looks fine (no tumors, no visible ulcers), but the engine isn’t running smoothly.
However, recent research suggests that many “functional” issues actually have organic causes—microscopic inflammation, enzyme deficiencies, or bacterial imbalances—that standard tests simply aren’t designed to find. Dr. Eva Alsheik, a gastroenterologist at Henry Ford Health, notes in a 2024 content update that when the gut is out of balance, it manifests in surprising ways, from skin irritation to anxiety, often signaling deeper issues than just “a sensitive stomach.”
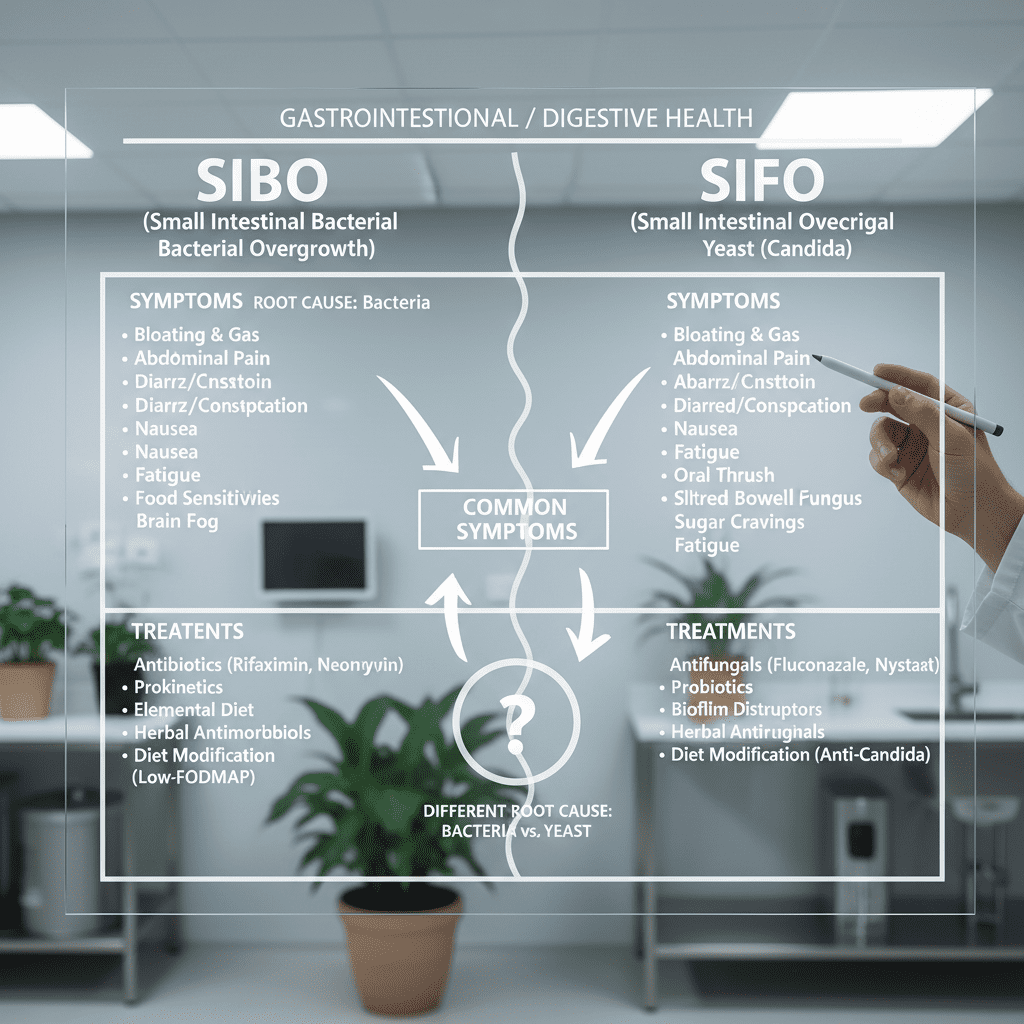
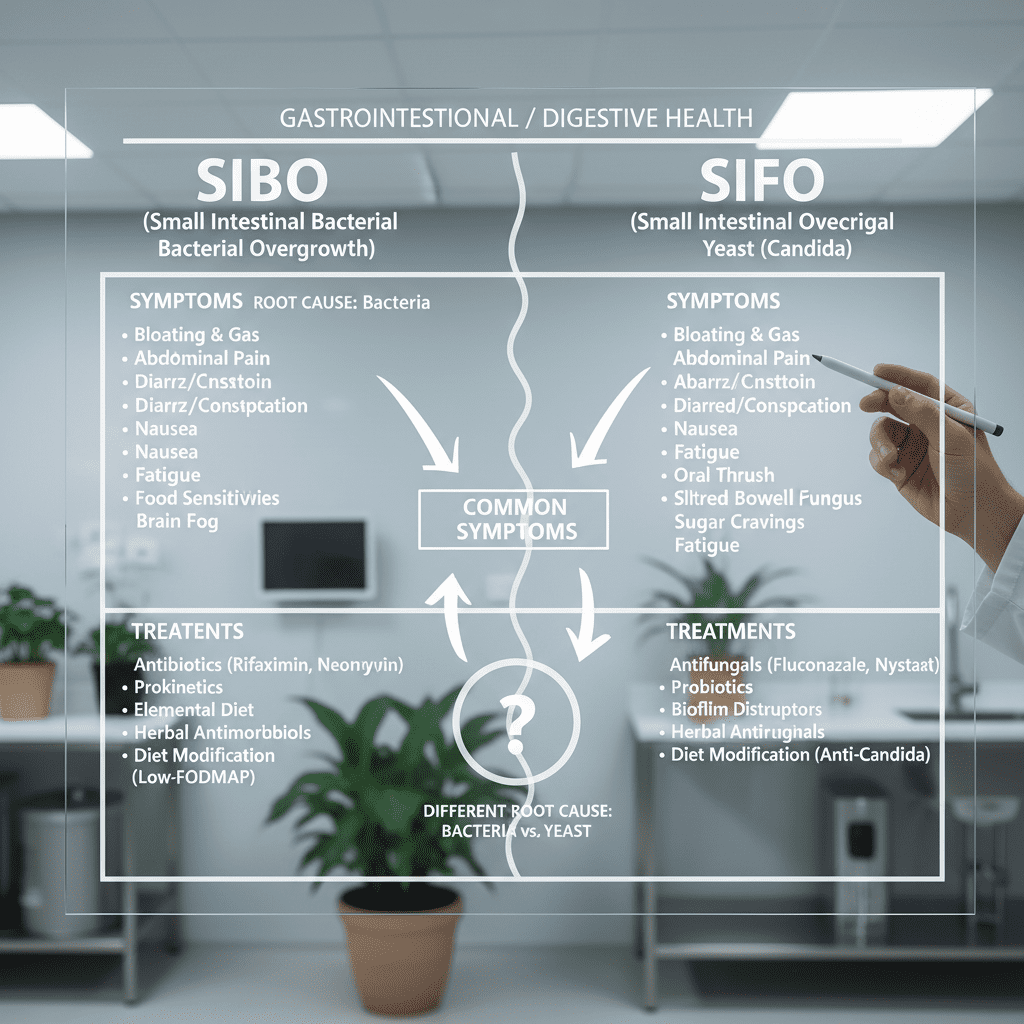
1. Small Intestinal Bacterial Overgrowth (SIBO)
If there is one condition that has exploded in awareness yet remains critically under-tested in standard primary care, it is SIBO. Your small intestine is supposed to be relatively clean, designed for nutrient absorption. The bacteria belong in the colon (large intestine). When those colon bacteria migrate upwards into the small intestine, chaos ensues.
The “90-Minute” Bloat
The hallmark of SIBO isn’t just bloating; it’s when the bloating happens. Because the bacteria are high up in your digestive tract, they start fermenting food before your body can absorb it. This typically results in severe distension about 90 minutes after eating. You wake up with a flat stomach, but by 4 PM, you can’t button your jeans.
Diagnostic Check: The Breath Test
A standard endoscopy won’t find this. You need a Lactulose or Glucose Breath Test. You drink a sugar solution and breathe into bags every 20 minutes. If hydrogen or methane levels spike early, it indicates bacteria are fermenting that sugar in the small intestine.
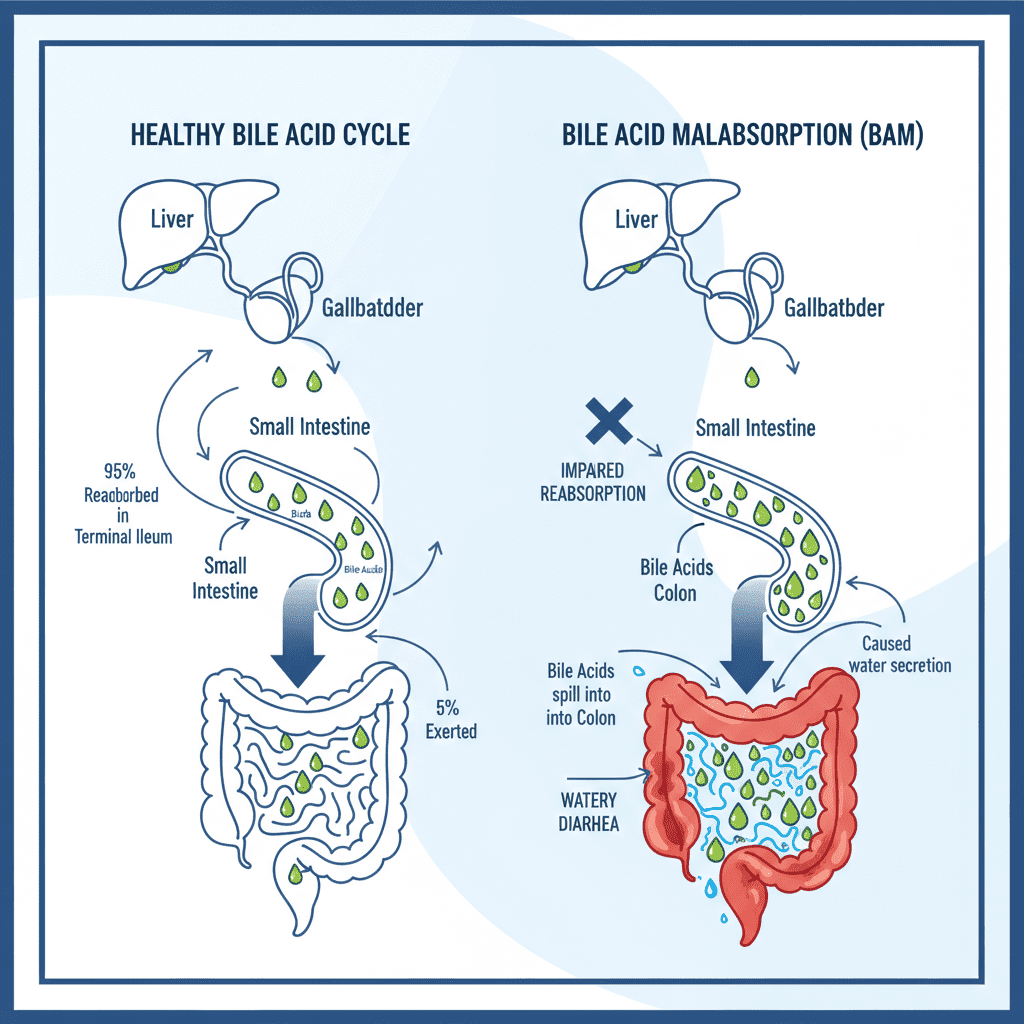
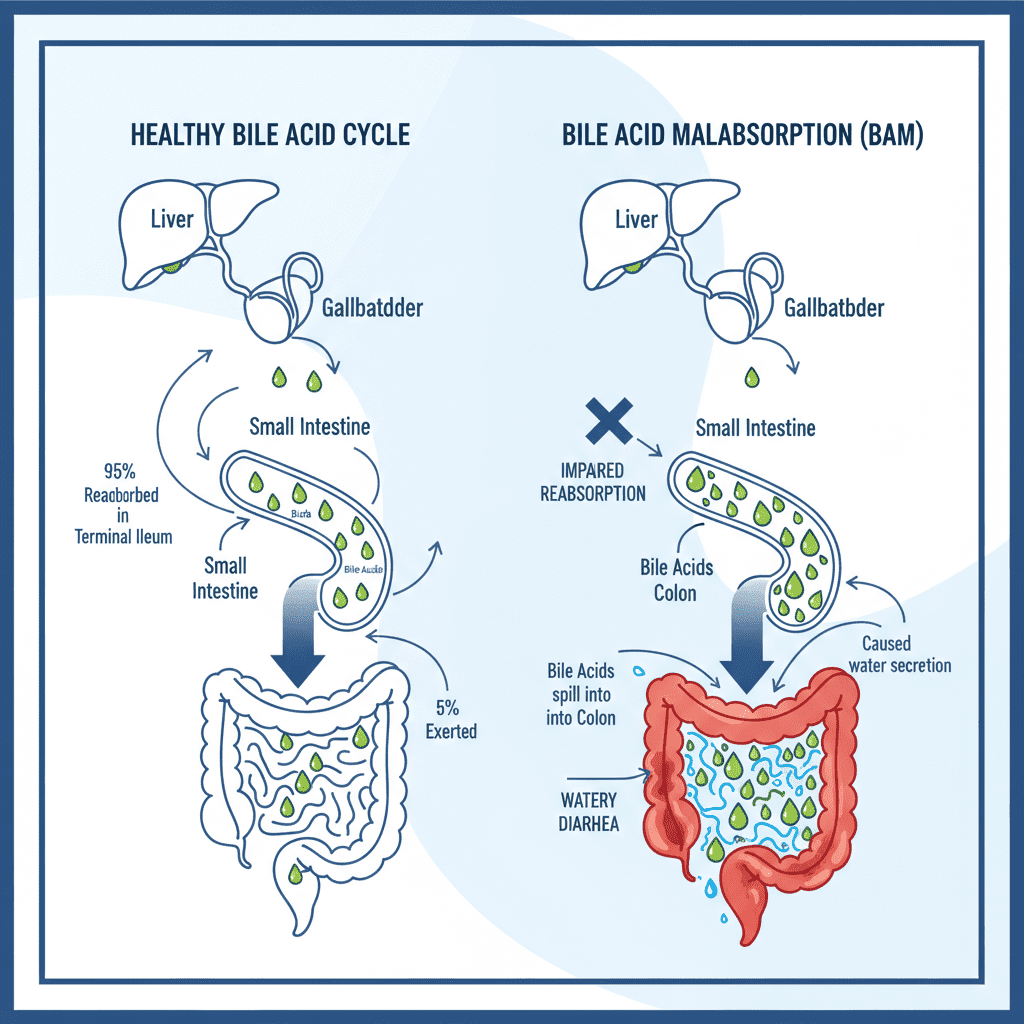
2. Bile Acid Malabsorption (BAM)
This is perhaps the biggest “blind spot” in modern gastroenterology. Bile acids are produced by the liver to digest fat. Usually, they are reabsorbed at the end of the small intestine. In BAM, they aren’t reabsorbed. They spill into the colon, irritating the lining and pulling in water.
The “Burning” Diarrhea
BAM is the number one cause of what doctors call “IBS-D” (IBS with Diarrhea). The symptoms are distinct: urgency, watery stools (often yellow), and a burning sensation. It often happens after gallbladder removal, but it can occur spontaneously.
Diagnostic Check: The SeHCAT Scan
The Gold Standard is the SeHCAT test, a nuclear medicine scan. However, it is not widely available in the US (more common in the UK/Europe). In the US, doctors often use a “therapeutic trial.” They prescribe a bile acid binder (like cholestyramine). If your symptoms stop within a few days, you have your diagnosis.
3. Exocrine Pancreatic Insufficiency (EPI)
We often think of the pancreas in relation to insulin and diabetes, but its other job is producing enzymes to break down food. If your pancreas is sluggish, you aren’t digesting, you’re just passing food through.
The “Floating” Stool
EPI is characterized by malabsorption, specifically of fats. Signs include unexpected weight loss, fatigue, and stools that are pale, oily, difficult to flush, or floating. This is medically known as steatorrhea.
Diagnostic Check: Fecal Elastase-1
This is an easy, non-invasive stool test. It measures Fecal Elastase-1. If the levels are low, your pancreas isn’t producing enough enzymes. The treatment involves taking enzyme replacement therapy (PERT) with meals.
4. Congenital Sucrase-Isomaltase Deficiency (CSID)
For years, doctors thought this was a rare genetic condition found only in infants. We now know that’s completely false. Many adults have a mild version where they lack the enzyme to break down sucrose (table sugar) and maltose (grains/starches).
The “Sugar” Trigger
If you get gas, bloating, and diarrhea specifically after eating fruit, candy, or starchy foods like bread and potatoes, this might be you. It mimics IBS perfectly but is strictly diet-dependent.
Diagnostic Check: Disaccharidase Assay
The most accurate test is a biopsy taken during an endoscopy specifically to measure enzyme levels (Disaccharidase assay). There is also a 13C-sucrose breath test that is becoming more available.
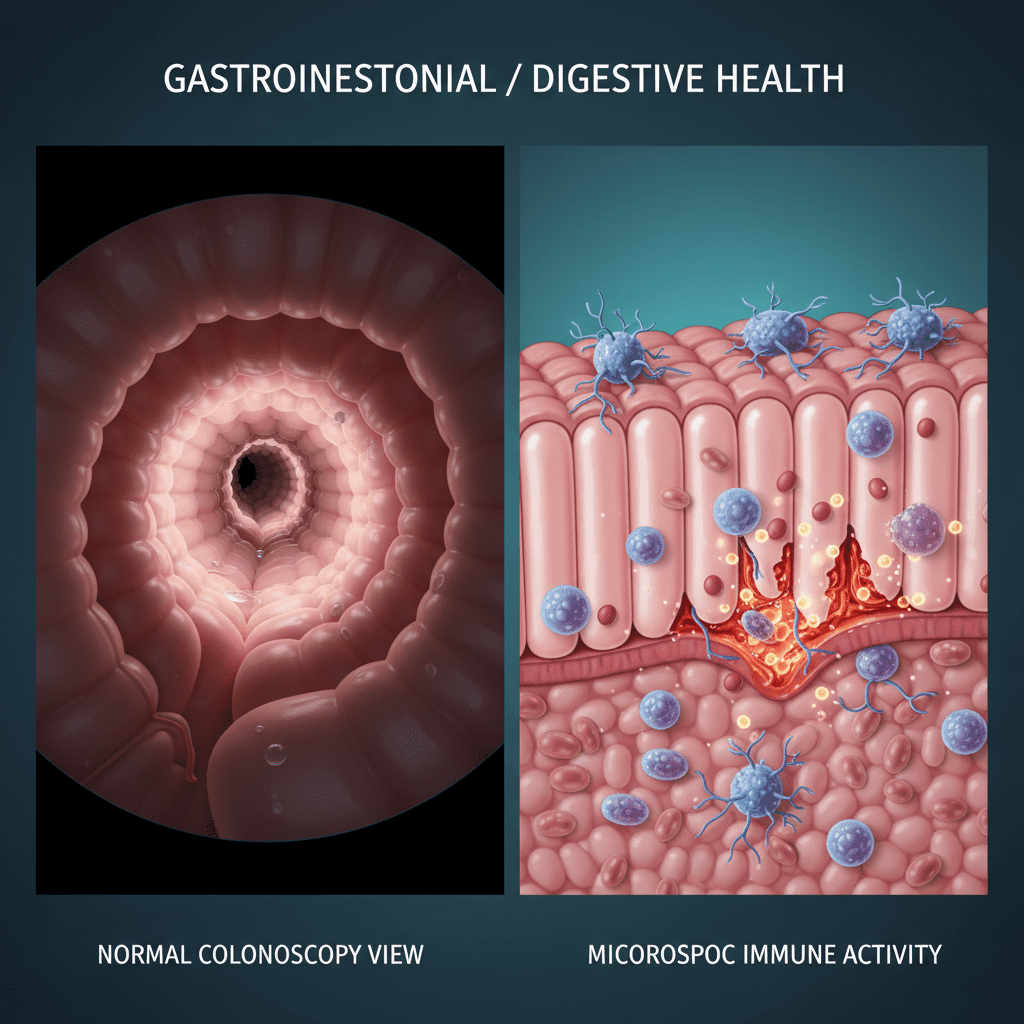
5. Microscopic Colitis
Standard colonoscopies look for polyps and cancer. If your colon looks “pink and healthy” to the naked eye, the doctor says you are fine. But they might be missing microscopic inflammation.
The “Invisible” Inflammation
Microscopic colitis causes chronic, watery diarrhea. It is most common in women and older adults, though I’ve seen it in younger populations too. It is often triggered by medications like NSAIDs (ibuprofen) or SSRIs.
According to a March 2024 report in GastroEndoNews, 10% of patients diagnosed with Microscopic Colitis remained unaware of their diagnosis 1 year later despite documentation, highlighting a massive gap in patient communication.
Diagnostic Check: Random Biopsies
You cannot diagnose this by looking. You must ask your gastroenterologist to take random biopsies from the colon during a colonoscopy, even if the tissue looks normal.
6. Mast Cell Activation Syndrome (MCAS)
This condition sits at the intersection of immunology and gastroenterology. Mast cells are allergy cells. In MCAS, these cells become hyper-reactive, releasing histamine and other chemicals in the gut.
When You Are Allergic to “Everything”
Patients with MCAS often feel like they react to almost every food. Symptoms aren’t just digestive; they include flushing, rapid heart rate, brain fog, and skin itching after meals. It’s often misdiagnosed as severe IBS or anxiety.
Diagnostic Check: Serum Tryptase
Diagnosis is tricky. It involves measuring serum tryptase (often normal unless in a flare) and urinary mediators (like N-methylhistamine). It usually requires an allergist or immunologist working with your GI doctor.
7. Abdominophrenic Dyssynergia (APD)
I find this condition fascinating because it is mechanical, not chemical. Patients often complain of looking pregnant by the end of the day. They take gas pills (simethicone), but it doesn’t help. Why? Because it’s not gas.
The “Mechanical” Bloat
In a healthy person, when the diaphragm pushes down (during breathing), the abdominal wall relaxes to make room. In APD, the diaphragm pushes down, but the abdominal muscles tighten instead of relaxing. This forces the contents of the abdomen outward. It’s a coordination failure.
The cure here isn’t diet—it’s physical therapy. Specialized biofeedback therapy can retrain the brain-gut muscle connection.
8. Silent Celiac Disease
Most people think Celiac disease means immediate, violent illness after eating bread. But “Silent Celiac” is dangerous precisely because it lacks those immediate gut symptoms.
The Damage Without the Pain
You might have unexplained iron-deficiency anemia, infertility, severe fatigue, or joint pain, but no stomach ache. Meanwhile, gluten is destroying your intestinal villi.
Diagnostic Check: tTG-IgA
A simple blood test (Tissue Transglutaminase IgA) is the first step. Crucial Note: You must be eating gluten daily for at least 6 weeks prior to the test for it to be accurate. Do not go gluten-free before testing.
9. Small Intestinal Fungal Overgrowth (SIFO)
Similar to SIBO, but instead of bacteria, it is yeast (usually Candida). This often occurs in people who have used proton pump inhibitors (PPIs) or frequent antibiotics.
When It’s Yeast, Not Bacteria
Symptoms are nearly identical to SIBO—bloating, brain fog, gas. However, SIFO patients won’t respond to standard antibiotics like Rifaximin; in fact, antibiotics might make them worse.
Diagnostic Check: Small Bowel Aspirate
Breath tests generally do not detect fungus. The gold standard is a small bowel aspirate during an endoscopy, where fluid is taken and cultured for fungi.
The “Hidden Gut” Diagnostic Checklist
This is your actionable tool. If you suspect your IBS diagnosis is incomplete, review this table. If a symptom profile matches yours, take the specific test name to your doctor.
| Primary Symptoms | Suspected Condition | Ask Your Doctor For… |
|---|---|---|
| Bloating 90 mins after eating; relief after passing gas. | SIBO (Bacterial Overgrowth) | Lactulose/Glucose Breath Test |
| Urgent, yellow, watery diarrhea; burning sensation. | BAM (Bile Acid Malabsorption) | SeHCAT Scan or Trial of Bile Acid Binders |
| Pale, floating, oily stools; weight loss. | EPI (Pancreatic Insufficiency) | Fecal Elastase-1 Stool Test |
| Gas/Diarrhea after fruits, sugar, or starch. | CSID (Sucrose Intolerance) | Disaccharidase Assay (Biopsy) or 13C-Sucrose Breath Test |
| Chronic watery diarrhea (esp. older adults/women). | Microscopic Colitis | Colonoscopy with Random Biopsies |
| Allergic reactions (flushing, itching) + gut pain. | MCAS (Mast Cell Activation) | Serum Tryptase & Urinary Mediators |
| Severe distension (“looking pregnant”) without gas. | APD (Dyssynergia) | Anorectal Manometry / Biofeedback Assessment |
| Anemia, fatigue, infertility (no stomach pain). | Silent Celiac | tTG-IgA Blood Test (while eating gluten) |
| Bloating not responding to antibiotics/low FODMAP. | SIFO (Fungal Overgrowth) | Small Bowel Aspirate (Endoscopy) |
FAQ: Your Burning Digestive Questions
What autoimmune diseases cause digestive issues?
Beyond Celiac disease, conditions like Hashimoto’s Thyroiditis, Sjögren’s syndrome, and Type 1 Diabetes are heavily linked to digestive issues. They can slow down motility (causing constipation/gastroparesis) or decrease stomach acid, paving the way for SIBO.
How do I know if I have SIBO or IBS?
IBS is a label for symptoms; SIBO is a cause. You can have both. However, 2024 studies show that up to 78% of IBS sufferers test positive for SIBO. The key differentiator is often the timing of the bloating (usually 90 minutes post-meal) and a positive response to antibiotics like Rifaximin.
Can Gastroparesis be mistaken for IBS?
Yes. Gastroparesis implies the stomach empties too slowly. New data from the American Foregut Society (Nov 2024) challenges traditional diagnostics, noting that 81.7% of gastroparesis patients have multiregional dysmotility. If you feel full after just a few bites of food (early satiety) and have nausea, ask for a Gastric Emptying Study.
Why do I have diarrhea after gallbladder removal?
This is the classic presentation of Bile Acid Malabsorption (BAM). Without a gallbladder to store bile, the liver drips it continuously into the intestines, overwhelming the system. It is highly treatable with bile binders.
Conclusion: Advocating for Your Gut
Navigating the medical system when you have invisible symptoms is exhausting. I know it feels easier to just accept the “IBS” label and live with the discomfort, but you deserve better. You deserve to eat without fear and live without pain.
Remember, you are the CEO of your own health. Doctors are the consultants. If a consultant isn’t giving you the answers you need, or if they dismiss your request for a specific test like Fecal Elastase or a SIBO breath test, it is okay to push back. It is okay to ask “Why not?” or to seek a second opinion from a motility specialist.
Use the checklist above. Print it out. Circle your symptoms. Take it to your next appointment. The difference between a lifetime of suffering and a cure might just be asking the right question.